What Are the Causes of Melasma?
Melasma is an acquired hyperpigmentation where there is a formation of dark brown patches and spots on the skin of the face and sun-exposed areas. When it is induced by pregnancy, it is called chloasma. It is more common in women, especially, those in their reproductive years, but about 10 % of the cases occur in men as well.
What Are the Clinical Features of Melasma?
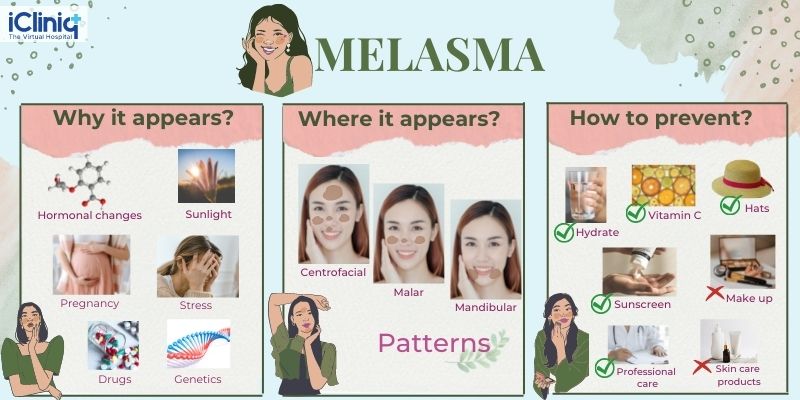
It is seen as irregular macular (flat, not raised) lesions of brown, blue-grey or brown-grey color that may occur in three patterns:
1. Centrofacial: involving the forehead, cheeks, upper lip, nose, and chin.
2. Malar pattern: involving the cheeks, and nose.
3. Mandibular pattern: involving the jaw.
Course of Melasma
Melasma usually runs a chronic course exacerbated by sunlight and artificial UVA and UVB light. Women have reported varying degrees of melasma during several pregnancies. Usually, melasma slowly resolves following childbirth or upon discontinuation of oral contraceptives.
What Are the Types of Melasma?
Based on Wood’s lamp examination of skin, melasma can be divided into:
- Epidermal: in this type melanin (pigment which synthesizes melanocytes responsible for the pigmentation of skin) deposition mainly occurs in the basal or suprabasal layer of the epidermis.
- Dermal: melanin-laden macrophages are found in the superficial and mid dermis.
- Mixed: melanin is found in both epidermis and dermis.
What Is the Treatment of Melasma?
- The individual should try to avoid sun exposure as much as possible and follow certain sun-protection measures like avoiding the midday sun (especially between 10 AM to 4 PM), seeking shade whenever possible, and wearing a broad-brimmed hat whenever out in the sun.
- Treatment of melasma during pregnancy or breastfeeding is not advisable.
- Sunscreen, usually broad spectrum with an SPF of more than 30, noncomedogenic, oil-free base should be preferred and should be applied 30 minutes before going out in the sun and repeated every fourth-hourly to obtain its full efficacy.
- Topical Hydroquinone cream 2 % should be used during night hours. This is suitable for superficial or epidermal melasma.
- A combination of Hydroquinone cream 2 % and Tretinoin/ Isotretinoin 0.025 % and Hydrocortisone cream 0.05 % (Kligman’s regime) is better for deeper or dermal melasma.
- Topical Azelaic acid, either alone or in combination with Isotretinoin can be used.
- Chemical peeling 35 to 70 % Glycolic acid (GA peel) or 10 to 15 % Trichloroacetic acid peel (TCA peel) can be used.
- Lasers like fractional CO2 and Q switched Nd YAG laser is, in recent times, the treatment of choice for resistant melasma.
For more information consult a melasma specialist online --> https://www.icliniq.com/ask-a-doctor-online/dermatologist/melasma













