What is Lung Transplantation?
A surgical approach of replacing a diseased or failing lung with a healthy lung taken from a donor is called lung transplantation. The donor's lung is taken from a dead individual, or in rare cases, a small portion can also be taken from a living donor. The lung transplantation procedure can be done for either one of the lungs or both lungs, depending on the individual's need for transplantation. Although lung transplantation possesses several complications, its improvement in terms of health and quality of life outweighs the complications. Since the demand for lung donors is high, lung transplantation is done only in reliable situations. Lung transplantation is recommended in cases only when medications and other treatments fail to respond and show any improvement. For example, it is not recommended in people with lung cancer because cancer recurrence in the healthy donor lung is highly possible.
What are the Types of Lung Transplantation?
Lung transplantation is primarily divided into three types, which includes the following:
1) Single Lung Transplant:
It is a surgical procedure in which a single damaged lung is replaced by a healthy donor lung. It is recommended to treat pulmonary fibrosis; however, it is not advised in people with cystic fibrosis as the infection spreads from the remaining lung to the healthy donor lung.
2) Double Lung Transplant:
It involves replacing both the failing lungs with a healthy lung from the donor. Cystic fibrosis and chronic obstructive pulmonary disease are the conditions in which a double lung transplant is done.
3) Bilateral Sequential:
It also involves replacing both, but only one lung is transplanted at a time.
Heart-Lung Transplant:
It is carried out in people with severe pulmonary hypertension in whom both the lungs and the heart are replaced with lungs and the heart removed from the donor.
When Is Lung Transplantation Needed?
A healthy lung is essential for getting the oxygen needed for survival. In a diseased lung or when the lung enters the end-stage, the effective functioning of the lungs is disturbed. Medication, special breathing devices, and other treatments help in improving lung function. If all of these fail to respond, a life-threatening situation arises. In such cases, lung transplantation is recommended. The following are the conditions where lung transplantation is recommended:
-
Chronic obstructive pulmonary disease, which includes chronic bronchitis and emphysema.
-
Idiopathic pulmonary arterial hypertension.
-
Cystic fibrosis.
-
Idiopathic pulmonary fibrosis.
What are the Risk Factors Of Lung Transplantation?
Lung transplantation holds several risk factors like organ rejection, risk of infection, and effects of the drugs. Of the above, the first two risks produce fatal complications.
Organ Rejection:
The first and foremost risk of lung transplantation is organ rejection. Our body's immune system detects the presence of foreign substances and produces a defense mechanism by attacking the donor organ. Despite finding the best possible match, the risk of organ rejection exists. It occurs soon after an organ is transplanted, and the risk reduces with time. In order to prevent organ rejection, immunosuppressant drugs are to be taken, which, in turn, have their own adverse effects.
Risk Of Infection:
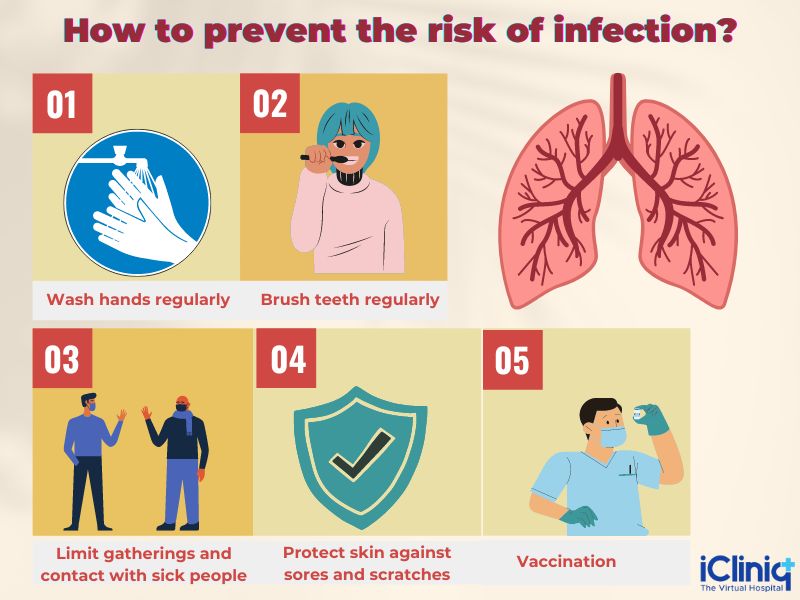
The immunosuppressants or the anti-rejection drugs taken lowers the body's immune response, making the body more prone to infections. Infections can be reduced by practicing the following:
-
Washing the hands regularly.
-
Regularly brushing the teeth.
-
Limiting gatherings and contact with sick people.
-
Protecting your skin against sores and scratches.
-
Getting appropriate vaccinations.
Adverse Effects of Immunosuppressants:
Just like any other drug, immunosuppressants or anti-rejection drugs have their own side effects.
Some common side effects include:
-
Abdominal problems.
-
Weight gain.
-
Development of facial hair.
In addition to the above-mentioned side effects, immunosuppressants also enhance the risk of developing or aggravates the following conditions:
-
Cancer.
-
Renal damage.
-
Osteoporosis.
-
Diabetes.
How Should You Prepare for Lung Transplantation?
After taking the adequate tests and having met the qualifying criteria, the name is added to the waiting list of donors. Waiting for a donor is a mental turmoil and depends on the following factors:
-
Blood group.
-
Severity of the condition.
-
The overall health of the individual.
-
Availability of matching donor lungs.
-
Geographic distance between the donor lung and the recipient.
It is necessary to provide the contact information to the hospital and be ready for transplantation at any time. It is always advisable to keep your bags packed at any time to be prepared to move to the hospital as the donor lung can be available at any time. In the meantime, laboratory tests and imaging tests are taken, and emotional counseling is given. The doctor also explains about the surgery and about how to prepare for the surgery.
How Is a Lung Transplantation Surgery Performed?
The surgery for lung transplantation is carried out under general anesthesia and will be painless. For breathing, a tube is inserted through the mouth into the windpipe. During the procedure, a cut is made in the chest, and the diseased lung is removed. Next, the donor’s lung is connected with the main airway and the blood vessel between that lung and heart. In some cases, for maintaining blood circulation, a heart-lung bypass machine may be used.
Once the surgery is completed, recovery usually involves a one to three-week stay in the hospital; however, the duration may vary for each patient. Immediately after surgery, the patient is kept in the Intensive care unit (ICU), and breathing is assisted with the help of mechanical ventilators. In addition, fluid drainage from the chest is aided with the use of tubes. Pain-relieving medications and immunosuppressants are given intravenously. Antibiotics, antiviral and antifungal drugs should be taken to prevent infections.
Regular and frequent check-ups are needed for the first three months, and the frequency of check-ups gradually reduces with time. Along with consultation with the treating pulmonologist, chest X-rays, laboratory tests, lung function tests, electrocardiogram (ECG), lung biopsy are done during every follow-up. Close monitoring of the symptoms of rejection and the adverse effects of immunosuppressant drugs is essential.
The below long-term adjustments should be followed:
-
Taking medications routinely without missing a dose, doing regular check-ups, performing tests to analyze lung function, and following lifelong care are essential.
-
Follow a healthy lifestyle by eating a nutritious diet, exercising regularly, and avoiding alcohol and tobacco.
-
Immunosuppressant medications should be taken to prevent the rejection of donor organs.
-
Emotional support to the patients is needed, which is done with the help of support groups and psychotherapy.
What is the Prognosis After Lung Transplantation?
About 80% of patients have no limitations of physical activity after the lung transplantation surgery. Also, after a period of one year, about 40% of people can start with their part-time work. Although the risk of rejection is reduced with time, the risk is not fully reduced, and the use of immunosuppressants is needed lifelong. However, the adverse drug reactions of the anti-rejection drugs are unavoidable and produce complications like diabetes, increasing the risk of contracting infections, kidney diseases, osteoporosis, etc.
The quality of life is eventually enhanced with lung transplantation; however, the survival rate is not much increased. About one-half of people have had a five-year survival after transplantation, and only a few people have crossed ten years after lung transplantation.
Conclusion:
To conclude, the risks of lung transplantation can be minimized by a healthy lifestyle and following the instructions of the treating pulmonologist and lung transplant team. Do not be anxious about the procedure and trust your body and your doctors.













