Introduction:
Women experience severe pain during labor. Women's right to request and receive labor pain was controversial – linked to religious belief in the nineteenth century. They viewed pain, including labor pain, as divine punishment, and interference was considered sinful. Nevertheless, many women in the modern community wish to have pain management either by analgesia or anesthesia during labor and delivery. Obstetric anesthesia combines art and science, dealing with the lives of the mother and the newborn. An obstetric anesthesiologist has now become an essential member of the peripartum care team, who works closely with obstetricians, perinatologists, neonatologists, and midwives to guarantee the pregnant woman receives the best possible care. Obstetrics is the only practice carried out daily in numerous centers in every corner of the world.
Obstetric anesthesiologists require in-depth knowledge and experience about the techniques and medications used for pain relief during labor. It is well known that the pain response varies from individual to individual. Physicians are committed to providing comfortable or at least tolerable labor and delivery. Many patients are tense and apprehensive at the onset of labor, although they may have little or no discomfort. The physician must be aware of the options for pain relief and respond to the patient's needs and wishes.
What Are the Types of Analgesia for Labor?
Almost all women experience severe labor pain during childbirth. This experience varies from individual to individual, and various methods to alleviate pain are chosen depending on the options given by the obstetrician.
What Are the Types of Labor Analgesia?
Labor analgesia can be of two types - Non-pharmacological and pharmacological methods.
Non-pharmacological Methods:
The administration is easy and has minimal side effects, but they are costly and time-consuming.
-
Some of the Non-pharmacological Methods Include- Transcutaneous electrical nerve stimulation (TENS), focus on breathing with meditation, modulation of temperature with spa techniques and hypnotherapy, and aromatherapy.
-
Transcutaneous Electrical Nerve Stimulation (TENS)- Used to reduce pain in labor, two electrodes are placed on the lower back on either side of the spine. The machine delivers small pulses of electric current to the body. The patient can alter the amount of current supplied to the electrodes as and when needed during contractions.
Pharmacological Methods:
Inhalation of nitrous oxide and halogenated gasses.
-
Nitrous Oxide Inhalation: Has been used in obstetrics for centuries; Etonox gas, a combination of 50 % nitrous oxide in oxygen, provides analgesia within 20 to 30 seconds of inhalation, with a maximum effect after about 45 seconds. It is straightforward to use, does not require supervision, and can be administered by the patient. However, it is not allowed to be self-administered by the patient. It causes drowsiness, disorientation, and nausea.
-
Inhalation of Halogenated Agents: Sevoflurane and Desflurane are used intermittently during labor for analgesia.
-
Systemic Analgesics: Analgesics (painkillers) such as Meperidine, Morphine, Fentanyl, Remifentanil, and patient-controlled analgesia (PCA) are used. PCA is useful in patients who are contraindicated to general anesthesia.
What Are the Regional Techniques for Labor Analgesia?
The most efficient form of labor analgesia is neuraxial analgesia, commonly used during labor and delivery with minimal side effects. These include traditional epidural, spinal, or combined spinal-epidural [CSE] analgesia, dural puncture epidural, and spinal analgesia.
-
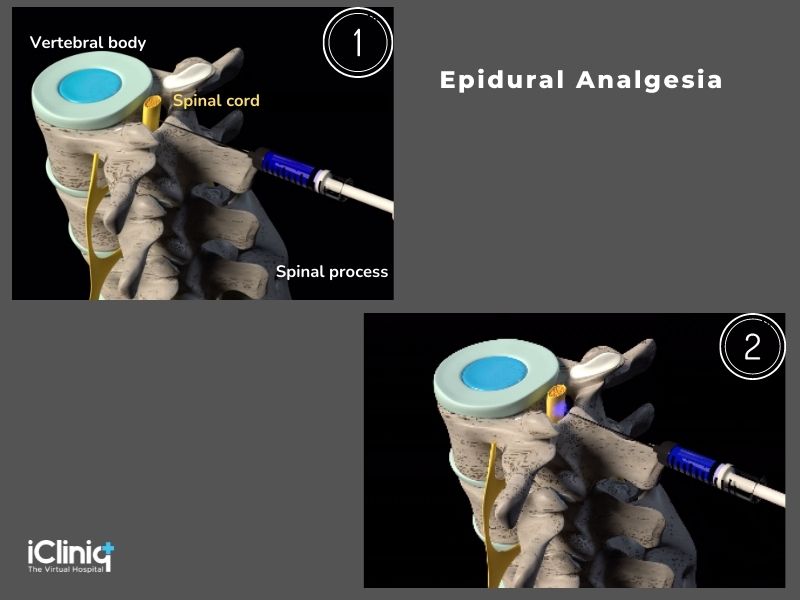
Epidural Analgesia:
In this technique, an epidural catheter of about a 19 to 29-gauge spinal needle is placed in the epidural space to administer analgesia. Maintenance of analgesia is possible with intermittent bolus injections, continuous infusion, or patient-controlled epidural analgesia (PCEA). The risk and benefits of epidural analgesia should be assessed and discussed with the patient before labor.
-
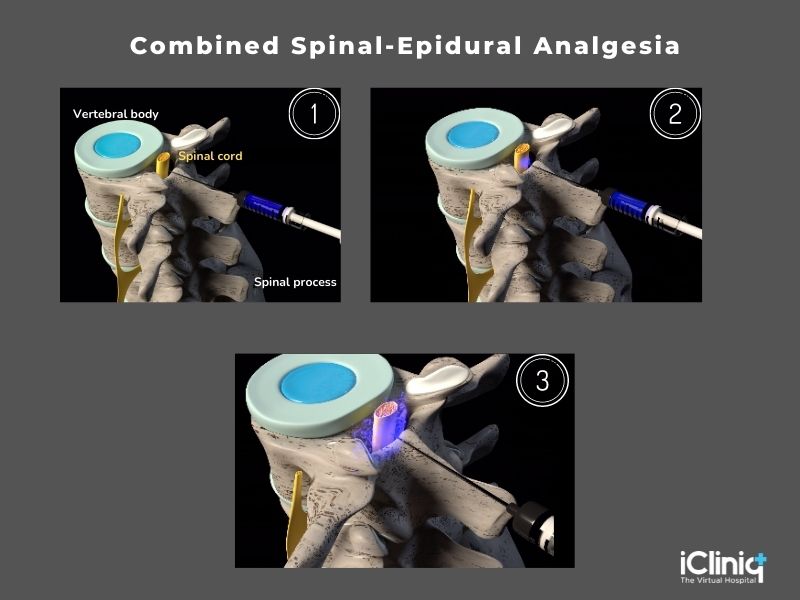
Combined Spinal-Epidural Analgesia (CSEA):
Combined spinal-epidural analgesia has gained popularity over the past few decades because of its fast-acting analgesic effect. However, this technique has a high risk of fetal bradycardia.
The epidural space is located with an epidural needle, and a spinal needle of 25 to 27 gauge is passed through the epidural needle, and the dura is punctured. Next, a local anesthetic, with or without opioids, is injected into the subarachnoid space. Next, the spinal needle is withdrawn, and a 19 to 20-gauge epidural catheter is introduced through the epidural needle to maintain subsequent doses.
-
Dural Puncture Epidural Technique (DPE):
This technique is effective only when a 26 gauge needle is used to puncture the dura-arachnoid space. This technique reduces the occurrence of frequent uterine contractions and hypertonia.
-
Continuous Spinal Technique:
This is used only in patients with a previous history of cardiac disease for whom the slow onset of anesthesia is preferred with adequate anesthetic coverage and quality.
-
Spinal Analgesia:
Smaller doses of local anesthetics Bupivacaine 5 to 8mg, with opioid (Fentanyl 10-25μg ), should be used to carry C-sections successfully. The anesthetic dosage is based on various factors such as height, weight, and age. Additional doses may be required during labor due to the low-dose regimen. The common side effects are arterial hypotension, spinal headache, nausea, and vomiting.
-
Caudal Analgesia:
Caudal analgesia is helpful in those patients whose labor pain has commenced already and who are suffering from pain. It provides the mother with relatively comfortable labor and painless delivery. The vitals and consciousness levels of the mother and the newborn are not altered. The patient can follow a regular diet and fluid intake, and thus there is no disturbance to the mother's metabolism. This method is not intended to be used in case of placenta previa, uterine inertia, and disproportion of the child to the placenta or any other underlying abnormalities.
What Are the Complications of Obstetric Anesthesia?
-
Hypotension: The decreased venous return to the heart due to the dilation and resistance of the vessels.
-
Fetal Bradycardia: Decreased preload following spinal anesthesia triggers the reflex that causes severe bradycardia (slow heart rate).
-
Post Dural Puncture Headache: The decrease of cerebrospinal fluid (CSF) volume, which causes cerebral hypotension, adenosine activation, and subsequent dilatation of cerebral arteries to enhance cerebral blood flow, is regarded to be the headache's primary cause. The cerebrospinal fluid (CSF) leakage is more during standing and sitting. Can minimize this leakage by lying. These headaches develop within the first 72 hours, and the patient develops neck stiffness, sensitivity to light, hearing loss, and continuous ringing in the ear.
-
Maternal Fever and Back Pain: These are due to the side effect of the spinal anesthesia given during childbirth. Fever lasts for about a few days after surgery, but back pain persists in some patients but gradually decreases.
-
Inadvertent Intravascular Injection of Local Anesthetics: Nerve injuries caused by regional anesthesia can be caused by direct nerve trauma, chemical injury, or compressive injury. Direct nerve trauma occurs during the placement of the central neuraxial block, in which needles and catheters can cause fluid to be injected. This immediate trauma results in transient neuritis that usually settles within three months to a year. These injuries can cause paraesthesia, loss of sensation, and muscle weakness in the affected nerve's distribution.
-
High or Total Spinal Anesthesia: Preoperative evaluation height of the block and quality is highly subjective, and techniques vary. According to anesthetist surveys, the modality of evaluation and the height of the block - the loss of cold or light response to stimuli is most frequently used. The most commonly mentioned block height that anesthetists focus on before a cesarean section is the bilateral loss of cold sensation below the fourth thoracic vertebrae bilaterally and the bilateral block to light touch to the fifth thoracic vertebrae.
-
Infection at the Site of Injection, Meningitis: Due to lumbar puncture for spinal anesthesia. This results in a break in the defense barrier of the central nervous system, thus predisposing to the risk of transmission of microbes or chemicals to meninges and subarachnoid space through bleeding caused by the puncture of the needle.
-
Peripheral Nerve Injury: Neuraxial blocks used during labor as a part of analgesia cause nerve injury. These nerve injuries are due to trauma to the nerve, chemicals, or due to any compression of the nerve.
Conclusion:
During labor, women experience severe pain throughout the lifespan of their life. Recent advances in managing pain during childbirth have drastically improved maternal and newborn outcomes. Improvements in neuraxial labor analgesia techniques, postpartum pain management strategies, and anticipation of maternal hypotension during cesarean delivery have improved the results. Obstetric anesthetics must be tailored for each patient to enhance patient safety and ease the process of labor. Morbidity and mortality have gradually decreased with the advances in the modern practice of obstetric anesthesia.











