An allergy is simply a hypersensitivity reaction of the body to various foreign substances referred to as allergens. Allergens, if found to be from within the patient's body itself, give rise to a group of disorders called as autoimmune diseases. Here we will be looking in particular at only allergic eye disorders.
How Is Allergy Caused?
Allergy is mainly caused by cells called mast cells and neutrophils in our bodily organs. These cells are part of a wider subfamily called white blood cells, the main function is the defense of our body. These cells contain substances like histamine, leukotrienes, prostaglandins, etc., whose main function is to alter blood flow characteristics within the blood vessels of our body. This change in blood flow coupled with a few mechanisms causes the changes basic to all allergies - redness, increase in temperature, and pain. The release of inflammatory mediators is effected by a process called degranulation, which is an important event as it triggers the inflammation cascade and sets the rest of the changes in motion.
Allergic Conjunctivitis
This refers to the allergic condition affecting the conjunctiva. The manifestations of this disorder include itching, watering, redness and blurred vision. The characteristic symptom of exposure to an allergen is often not seen in a majority of cases, the main clue is itching and an urge to rub. This is a universal symptom seen in most patients of allergic conjunctivitis.
The heart of the problem lies in the symptom of rubbing. Rubbing causes degranulation of mast cells and neutrophils, worsening the problem of allergy. Hence, it is imperative that the patient avoids rubbing in spite of the uncontrollable urge to do so. Rubbing sets up a vicious cycle, such that the more the patient rubs, the more the itching and severity of the allergy.
Treatment
There are several treatment modalities, each with its own mechanism of action and side effect profile. The main determinant of the type of treatment given is the severity of the allergic response. The other determinants being age, duration of the allergy and intraocular pressure.
The most commonly used modalities include eyedrops of the following types -
a) Steroids - these drugs act by suppressing the immune responses of our body. So, there will be less severe inflammation and hence less damage to tissues. Steroids, although not the first line of treatment in most cases is the most potent drug in allergy treatment.
A few notable examples are Loteprednol, Prednisolone, Difluprednate, and Fluorometholone. Although having the best results in a short time, the steroids are notorious for causing side effects such as glaucoma, cataract formation, increased susceptibility to infection. This basic dictum applies even within the class of steroids - more potent the steroid, the more the side effects. Hence it becomes a matter of balancing side effects with the potency of the treatment. Another drawback is that the drug cannot be stopped at once but needs to be slowly tapered and stopped.
b) Mast cell stabilizers - these drugs act by preventing the degranulation of mast cells, which are the key mediators of inflammation. These drugs are usually considered the main drugs to control allergy. The downside of these drugs is that they are not as potent as steroids and have a period of waiting before they start to act. The advantages being that it is safer than steroids and does not have to be tapered.
c) Cyclosporine - these drugs act by inhibiting the actions of mediators of inflammation such as interleukin-2, is currently being used more than ever before because of its very minimal side effect profile, especially in children who will need a potent drug for long periods of time. Its limitations are that it needs a long time before it begins action. This latent period makes the cost of therapy significant and quite unsustainable for the not so well off patients.
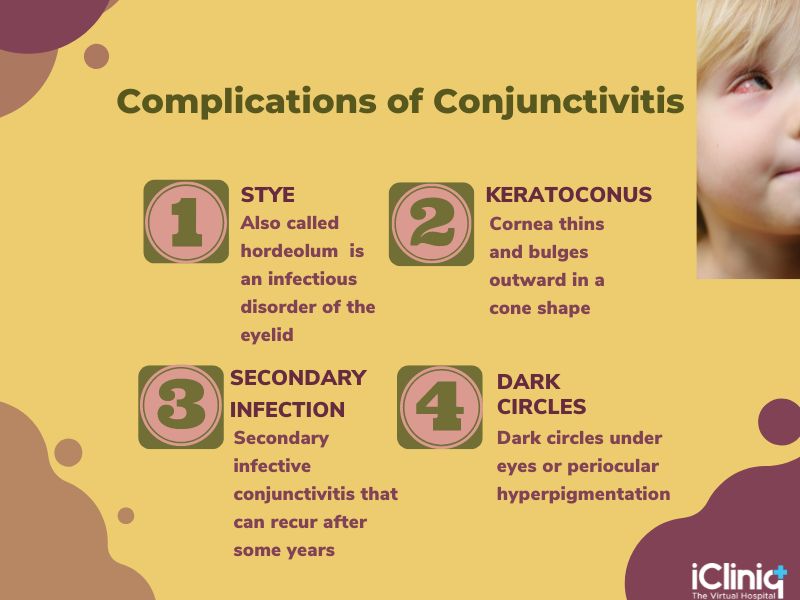
Complications in Long-Standing Allergic Conjunctivitis
- Stye.
- Keratoconus.
- Dark circles.
- Secondary infective conjunctivitis.
Hence allergic conjunctivitis, although a simple problem, can cause quite a bit of trouble. A good follow up with your ophthalmologist and proper adherence to treatment is recommended.
For more information consult an eye care ophthalmologist online --> https://www.icliniq.com/ask-a-doctor-online/eye-care-ophthalmologist













