Introduction
Hepatotoxicity of the drugs is not observed during clinical trials. Instead, it is discovered when prescribed to the public, and its adverse effects are noticed after some time. It is difficult to find the causes of drug hepatotoxicity as the symptoms are similar to the biliary disease. The liver is the primary site of drug metabolism and an important target for drug-induced injury. Pre-existing liver disease may affect the liver’s capacity to metabolize drugs, and unexpected toxicity may occur when patients with liver disease are given drugs in normal doses. Some drugs should be avoided in patients with cirrhosis as they can exacerbate known complications of cirrhosis. The possibility of undiagnosed underlying liver injury should always be considered in patients exhibiting unexpected symptoms following drug exposure.
What Is Hepatotoxicity?
Liver damage due to drugs or chemicals in them resulting in poor liver functioning is called hepatotoxicity. Therefore, drug toxicity should always be considered in patients with acute liver failure, jaundice, or abnormal liver biochemistry. Drug-induced liver injury can be classified into three types based on clinical presentation:
-
Hepatocellular Injury - An injury that causes damage to the liver cells.
-
Cholestatic Injury - Occasionally, permanent bile duct loss (ductopenia) follows a cholestatic drug reaction due to Co-amoxiclav, resulting in chronic cholestasis with persistent systems such as itching.
-
Mixed - An injury that has both the feature of hepatocellular injury and cholestatic injury.
What Are the Causes of Drug-Induced Hepatotoxicity?
The following are the drugs that cause hepatotoxicity:
-
Drugs such as Chlorpromazine and high dose of estrogen cause cholestasis.
-
Non-steroidal anti-inflammatory drugs (NSAIDs), Co-amoxiclav, and statins toxicity result in cholestatic hepatitis (liver inflammation).
-
Rifampicin and Isoniazid toxicity results in acute hepatitis.
-
Amiodarone toxicity causes non-alcoholic steatohepatitis.
-
Busulfan and Azathioprine drug toxicity results in obstruction of venous outflow.
-
A high dose of Methotrexate causes liver fibrosis.
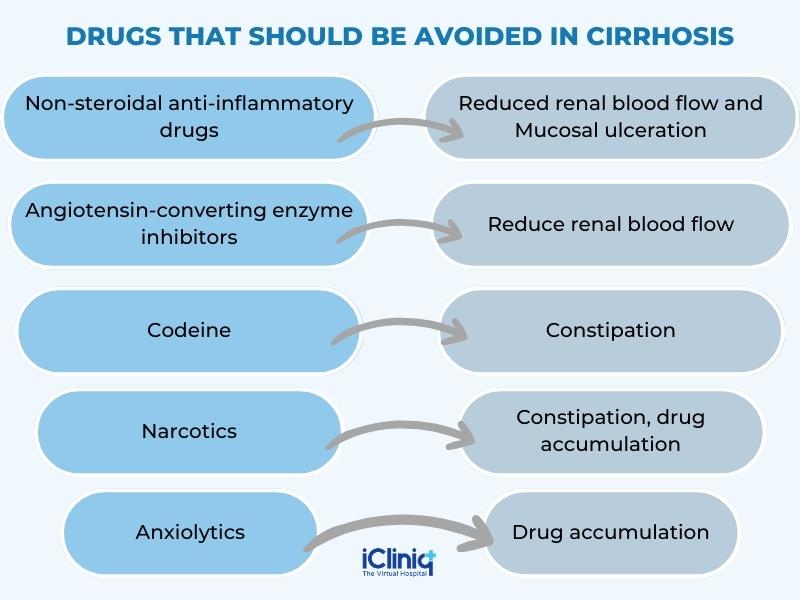
Co-amoxiclav is the most common antibiotic to cause abnormal LFT, but unlike other antibiotics, it may not produce symptoms until 10 to 42 days after it is stopped. Some drugs that should be avoided in patients with cirrhosis, as they can exacerbate known complications of cirrhosis, are:
What Are the Types of Liver Injury?
Different histological patterns of liver injury may occur with drug injury. Following are the types of liver injury -
1. Cholestasis - Pure cholestasis (selective interference with bile flow in the absence of liver injury) can occur with estrogens.
-
Cholestasis is common when a high concentration of estrogen (50 microgram/day) is used as a contraceptive. However, the current oral contraceptive pill and hormone replacement therapy can safely be used in chronic liver disease.
-
Drugs like Chlorpromazine and antibiotics such as Flucloxacillin cause cholestatic hepatitis, characterized by inflammation and canalicular Injury.
-
Anabolic glucocorticoids used by bodybuilders may also cause cholestatic hepatitis.
-
In some cases, non-steroidal anti-inflammatory drugs, and cyclo-oxygenase-2 (COX-2) inhibitors, there is overlap with acute hepatocellular Injury.
2. Hepatocyte Necrosis -
-
Many drugs cause acute hepatocellular necrosis with high serum transaminase concentration; Paracetamol is the best known for causing hepatoxicity.
-
Inflammation is not always present but accompanies liver injury necrosis due to Diclofenac (an NSAID) and Isoniazid (an anti-tuberculosis drug).
-
Granulomas may be seen in liver injury following the use of Allopurinol.
-
Acute hepatocellular necrosis has also been described following the use of several herbal remedies, including germander and comfrey.
-
Recreational drugs, including cocaine and ecstasy, can also cause severe acute hepatitis.
3. Steatosis -
-
Microvesicular hepatocyte fat deposition due to the direct effect on mitochondrial beta-oxidation can follow exposure to Tetracycline and Sodium valproate.
-
Macrovesicular hepatocyte fat deposition has been described with Tamoxifen and Amiodarone toxicity.
4. Vascular Lesions -
-
Drugs such as the alkylating agent used in oncology can damage the vascular endothelium and lead to hepatic venous outflow obstruction.
-
A chronic overdose of vitamin A can damage the sinusoids and trigger local fibrosis, resulting in portal hypertension.
5. Hepatic Fibrosis -
-
Most drugs cause reversible liver injury, and hepatic fibrosis is uncommon.
-
Methotrexate can cause acute liver injury when it is started and can lead to cirrhosis when used in high doses over a long period.
-
Risk factors for drug-induced hepatic fibrosis include pre-existing liver disease and a high alcohol intake.
What Are the Symptoms of Drug-Induced Hepatotoxicity?
The mechanism of hepatotoxicity is of two types:
-
Intrinsic or dose-dependent.
-
Idiosyncratic or unpredictable.
The presence of jaundice indicates the most severe form of liver damage. The symptoms are directly proportional to the toxicity dose, and symptoms may subside once the drug is withdrawn. Symptoms of hepatotoxicity are as follows:
-
Severe itching.
-
Jaundice.
-
Weakness.
-
Abdominal pain.
-
Hepatomegaly (enlarged liver).
-
Dark stools.
-
Dark urine.
-
Nausea.
-
Pruritus (itching of the skin).
-
Fever.
-
Rashes.
-
Eosinophilia.
-
Increase in weight.
-
Swelling in feet and hands.
How to Diagnose Drug-Induced Hepatotoxicity?
Drug toxicity should always be considered a differential diagnosis of the presenting patient with acute liver failure, jaundice, or abnormal liver biochemistry. The most common picture is mixed cholestatic hepatitis. The presence of jaundice indicates severe liver damage. Although acute liver failure can occur, most drug reactions are self-limiting, and chronic liver damage is rare.
The key to diagnosing acute drug-induced liver disease is to take a detailed drug history, looking for a temporal relationship between drug exposure and the onset of liver abnormality (bearing in mind that liver injury can frequently take weeks or even months to develop following the exposure. The following are the keys to diagnosing drug-induced hepatotoxicity;
-
A tabulation of the drug taken, either prescribed or self-administered.
-
After the drug history, establish whether hepatotoxicity is reported in the literature.
-
Relate the time the drugs were taken to the onset of illness, four days to 8 weeks (usual).
The following are the ways to diagnose drug-induced hepatotoxicity;
-
Liver Function Test (LFT) - Abnormal LFT often takes weeks to normalize following drug-induced hepatitis, which may be months before they normalize after cholestatic hepatitis.
-
Blood Test - Complete blood count will show infection and allergy if present. Jaundice is the most common feature of hepatotoxicity, and bilirubin levels can confirm it.
-
Alanine Aminotransferase Test - Large increase in aminotransferase activity favors hepatocellular damage.
-
Biopsy - A liver biopsy should be considered if there is suspicion of pre-existing liver disease or if the blood tests failed to improve when the suspect drug is withdrawn.
How to Treat Drug-Induced Hepatotoxicity?
Where the drug-induced liver injury is suspected or cannot be excluded, the potential culprit drug should be discontinued unless it is impossible to do so safely. The drugs should be discontinued only after consulting with the doctor. If the toxicity is severe, then patients should be hospitalized.
-
The suspected drug should be withdrawn.
-
Glucocorticoids can be given for the symptomatic treatment of hepatitis.
-
L-creatinine is given for Valproic acid overdose.
-
N-acetyl-cysteine is the treatment for Acetaminophen toxicity.
-
Anti-histamine can be given for symptoms such as itching or rashes (pruritis).
-
Over-the-counter drugs can be given for fever.
Conclusion
Drug-induced hepatotoxicity can be fatal if left untreated or if the use of suspected drugs is to be continued. Generally, the recovery of the patients is 90 percent after the discontinuation of the suspected drugs. Liver transplantation is the last resort to treat liver injury. Many drugs are listed as toxic, so it is important to give accurate drug history to the doctor if hepatotoxicity is suspected. People should consult a doctor as soon as they observe symptoms of hepatotoxicity.












