Overview:
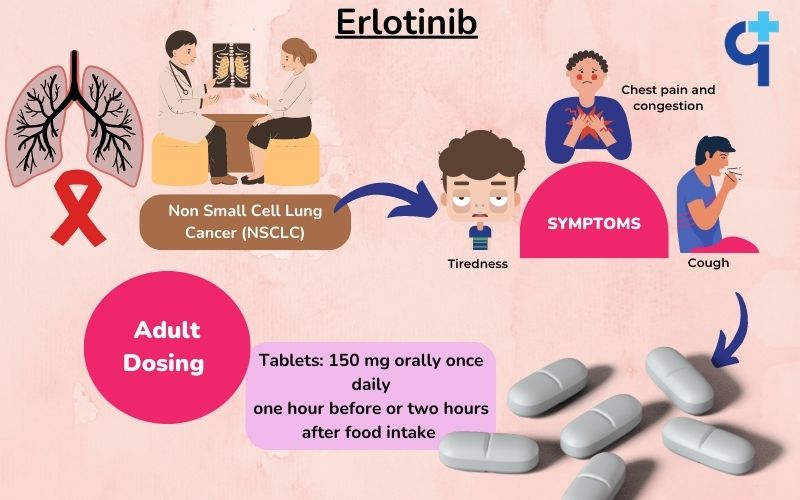
Erlotinib is an immunosuppressant drug approved for treating adult non-small cell lung cancer (NSCLC). It is an epidermal growth factor receptor (EGFR) inhibitor that inhibits the autophosphorylation of tyrosine kinase leading to prevention in cell signaling, survival, and proliferation. Erlotinib is available in tablet form and has three doses 25 mg, 100 mg, and 125 mg.
Erlotinib is also used for the treatment of pancreatic cancer. The U.S Food and Drugs Administration approved Erlotinib on October 18, 2016, to treat NSCLC for people with specific EGFR mutations. The active ingredient in the Erlotinib tablet is Erlotinib Hydrochloride. Sun exposure may cause skin reactions while taking Erlotinib; therefore, using sunscreens or sun-protection hats is recommended. The safety of Erlotinib in children is not yet known.
How Does Erlotinib Work?
The tyrosine kinase function of the epidermal growth factor receptor (EGFR) is reversibly inhibited by Erlotinib, which prevents the autophosphorylation of tyrosine residues linked to EGFR and reduces the signaling, survival, and proliferation of tumor cells.
Uses:
Erlotinib is indicated for use in the following conditions:
-
Treatment of people with locally advanced or metastatic (spread to other organs) non-small cell lung cancer (NSCLC) who have received four cycles of platinum-based chemotherapy as first-line and for those whose cancer has not progressed.
-
The management of non-small cell lung cancer that has spread locally or far after at least one chemotherapy regimen failed.
Dosage:
Erlotinib is available in tablet form and should be taken as per the doctor’s instructions.
Listed below are the things to be followed while taking Erlotinib tablets:
-
The National Institute of Occupational Safety and Health (NIOSH) recommends wearing gloves while administering the tablet.
-
Erlotinib is to be administered on an empty stomach, at least 1 hour before or 2 hours after food.
-
The tablet should not be taken along with drugs belonging to the proton pump inhibitors class (e.g., Pantoprazole, Esomeprazole, Omeprazole, etc.) as it can raise the gastric pH.
-
If an H2 blocker (such as Ranitidine) is to be taken, Erlotinib should be administered at least two hours before the next dose and at least 10 hours after the previous dose.
-
If an antacid is required, provide Erlotinib several hours after taking an antacid.
Warning:
-
Hypersensitivity Reactions: This drug has sometimes been associated with allergic or hypersensitivity reactions. Itching and symptoms like swollen lips, face, or tongue have been noted. Medical help is required if these symptoms arise.
-
Skin Reactions: If symptoms like blistering or bullous appear, they may indicate a serious condition called Stevens-Johnsons syndrome. In such cases, report to the doctor immediately for emergency intervention.
-
Gastric Conditions: People with gastric conditions like peptic ulcers, or those on therapy with drugs like non-steroidal anti-inflammatory agents (NSAID), corticosteroids, or chemotherapy agents including, Vincristine, Vinblastine, may experience symptoms of gastric perforation, which requires medical attention.
-
Liver Diseases: Symptoms related to the feces and urine, such as dark urine, light stools, upper abdominal pain, yellowish discoloration of the skin and nails, etc., indicate liver damage that may be caused by Erlotinib that requires medical care.
-
Eye Problems: Erlotinib can cause symptoms like decreased tear production, eye pain, abnormal growth of eyelashes, and inflammation of the eye, which can point to the formation of ulcers in the eye. These symptoms should be immediately reported, and in some cases, drug discontinuation may be required.
-
Lung Diseases: If symptoms like shortness of breath, cough, or fever arise, report to the doctor for an examination for necessary action.
-
Pregnancy: Avoid the use of the drug during pregnancy.
For Patients:
What Is Non-small Cell Lung Cancer?
Non-small cell lung cancer (NSCLC) is one of the most common forms of lung cancer, with a yearly incidence rate of nearly 100 per 100,000 people in the United States. NSCLC accounts for about 80% of all lung cancers and is commonly seen among men and smokers. Treatment options for NSCLC include surgery to remove the tumor, chemotherapy to kill cells that have become resistant to treatment, radiation therapy to kill remaining cells that other treatments haven’t killed, and targeted therapies that aim to block the development of resistance to chemo. Survival rates are highest for those diagnosed in their early stages, with a five-year overall survival rate of about 80%.
What Are the Causes of NSCLC?
There are many possible causes of NSCLC, but genetics and smoking play a big role in who gets it. Smoking causes changes in the genes that lead to NSCLC. Changes in certain genes may also make it more likely for NSCLC cells to be able to grow and spread. Some people have a genetic basis more likely to develop NSCLC, even if they don't smoke. Other risk factors for NSCLC include long-term exposure to air pollution, infection with certain viruses, and exposure to chemicals like asbestos or benzene. Also, some cases of NSCLC can be caused by tumors elsewhere in the body that travel to the lungs.
What Are the Symptoms of NSCLC?
Signs and symptoms of NSCLC may include a cough that does not go away or gets worse over time, shortness of breath with chest pain (angina), easy fatigue, and weight loss. If these signs or symptoms do not go away after seeing the doctor, talk to them about having a biopsy or a scan for the diagnosis.
Learn More About Erlotinib:
When and Why to Take Erlotinib?
Erlotinib is prescribed for NSCLC and has also been approved for treating pancreatic cancer. It is an immunosuppressive therapy that prevents the proliferation of cancerous cells.
How Effective Is Erlotinib?
A twelve-month study has shown that Erlotinib given after chemotherapy showed a 29 % reduction in the disease progression in NSCLC.
Things to Inform The Doctor Before They Prescribe Erlotinib:
Inform the doctor if any of the below-mentioned conditions are present:
-
A history of allergic reactions to any drugs.
-
Talk to the doctor if you're taking any other medications that could affect how much Erlotinib is in the blood or affect how it works (such as antifungals like Ketoconazole, protease inhibitors, antibiotics (Erythromycin, Carithromycin), Phenytoin, Carbamazepine, barbiturates, St. John's Wort, etc.
-
Erlotinib may increase the chances of bleeding if the patient is also using an anticoagulant (a medication that helps to prevent thrombus or blood clotting, such as Warfarin). Speak with the doctor; he will need to perform blood tests for close monitoring.
-
Inform the doctor if the patients wears contact lenses and have a history of eye issues, such as very dry eyes, corneal inflammation, or corneal ulcers.
Starting Erlotinib:
How to Take Erlotinib?
-
Erlotinib is to be administered on an empty stomach at least one hour before or two hours after food.
-
Take the medication exactly as advised by the doctor.
-
In case of any doubt, contact the doctor or the pharmacist.
-
The starting dose of Erlotinib for NSCLC is 150 mg. It is important to take regular follow-ups as scheduled and inform the doctor of any side effects.
Things to Do After Taking Erlotinib:
Inform the doctor if the following symptoms arise:
-
Experience unexpected breathing problems accompanied by a cough or fever; the doctor may need to treat you with additional medications while stopping your Erlotinib treatment.
-
Experience diarrhea; the doctor may prescribe an anti-diarrheal medication (such as Loperamide);
-
Get severe or ongoing diarrhea, nausea, lack of appetite, or vomiting; tell the doctor immediately as they may need to stop Erlotinib treatment or require medical attention.
-
Experience excruciating abdominal discomfort, blistering, or skin peeling.
-
Experience acute or worsening eye redness and pain, increased eye watering, impaired vision, and sensitivity to light; immediately notify the doctor or nurse as the patient might require urgent care.
-
If the patient is taking drugs belonging to statin class and have inexplicable cramps, weakness, or soreness in the muscles. The treatment may need to be stopped or interrupted by the doctor.
Look Out for Side Effects:
Side effects or adverse effects are common with chemotherapy treatment. Immediately report to the doctor if any of these side effects appear.
-
Rash, which may occur or worsen in sun-exposed areas.
-
Numbness in the extremities.
-
Difficulty in breathing.
-
Nausea.
-
Headache.
-
Mouth irritation.
-
Depression.
-
Abnormal blood tests for liver function.
-
Stomach pain.
-
Loss of appetite.
-
Decreased weight.
-
Indigestion.
-
Flatulence.
-
Itching.
-
Dry skin.
-
Loss of hair.
-
Tiredness.
-
Fever.
Common Side Effects
-
Bleeding from the stomach or the intestines.
-
Bleeding from the nose.
-
Cracked skin.
-
Inflammatory reactions around the fingernail.
-
Infection of hair follicles.
-
Acne.
Uncommon Side Effects
-
Overgrowth of eyelashes.
-
Excess body and facial hair like in men.
-
Eyebrows change.
-
Brittle and loose nails.
Dietary Alterations:
Avoid taking grapefruit or grapefruit juices while taking Erlotinib, as it may alter the drug's efficacy. Erlotinib should be taken either one hour before a meal or two hours after or on an empty stomach. The medication should be taken at around the same time each day as instructed by the physician.
What Should Be Done if a Dose Is Missed?
It is important to strictly comply with the treatment schedule for the drug to work efficiently. However, immediately report a dose to the doctor or pharmacist if a dose is missed. Avoid taking double doses to catch up for a missed dose.
What Should Be Done to Treat Erlotinib Overdose?
There is only limited data regarding overdosing with Erlotinib. Overdosing can cause the appearance of symptoms like diarrhea, rash, and the elevation of liver enzymes. If this happens, immediately contact the emergency department of a nearby hospital for immediate medical intervention.
How to Store the Erlotinib Tablet?
-
Keep the drug in a dry and cool place, away from children or pets.
-
Do not take Erlotinib tablets after the expiration date, which will be given on the back of the carton and blister. The last day of that month is referred to as the expiry date.
-
Never dispose of medications in wastewater or household garbage. Find out from the pharmacist how to dispose of expired medications.
Avoid Self-Medication:
Erlotinib is a very potent drug that affects cell growth and proliferation and is only available on a doctor's prescription. Therefore, taking this medication without a prescription can have several severe adverse effects. This medication should not be taken on the recommendation of another patient or with someone else's prescription as a drug.
For Doctors:
Indication:
-
For non-small cell lung cancer, a metastatic disease with EGFR exon 19 deletions or exon 21 substitution mutations, first-line maintenance.
-
Second- or greater-line treatment after progression following at least one prior chemotherapy regimen.
Dosing:
Other Dosing Considerations:
-
Renal Toxicity, Grade 3 or 4: Discontinue Erlotinib until the condition has returned to normal or is of Grade 1 or less severity, then restart it with a daily dose reduction of 50 mg.
-
Hepatic Impairment or Preexisting Biliary Obstruction: In case of a three-fold rise in transaminases or a two-fold rise in total bilirubin over baseline impairment: Erlotinib should be stopped until the severity has decreased to Grade 1 or less, and then restarted at a daily dose reduction of 50 mg. If there is no noticeable improvement or resolution after three weeks, stop using the drug.
-
Hepatotoxicity: Erlotinib should be stopped until the severity has decreased to Grade 1 or less and then restarted at a daily dose reduction of 50 mg. If there is no significant improvement after three weeks, stop using the medication.
-
Concurrent Cigarette Smoking or Concomitant Use of Moderate CYP1A2 Inducer: Erlotinib dosage should be increased by 50 mg increments every two weeks, up to a daily maximum of 300 mg. If smoking is stopped, decrease Erlotinib dosage right away to 150 or 100 mg per day.
Mechanism of Action:
Both healthy and malignant cells express the epidermal growth factor receptor (EGFR) on their cell surfaces. Regardless of the presence of EGFR mutations, this receptor's signaling activity contributes to the survival and proliferation of some tumor cells. Erlotinib inhibits the kinase activity of the EGFR in a reversible manner, halting the autophosphorylation of the receptor's associated tyrosine residues and obstructing subsequent downstream signaling. Erlotinib has a higher affinity for the EGFR exon 21 (L858R) mutation or exon 19 deletions than it does for the wild-type receptor. The inhibition of other tyrosine kinase receptors by Erlotinib is not completely understood.
Pharmacodynamics:
Other than the mechanism, the drug's pharmacodynamics data is unavailable.
Active Ingredients:
The active ingredient present in Erlotinib tablets is Erlotinib Hydrochloride.
Inactive Ingredients:
The inactive ingredient present in Erlotinib tablets are;
Tablet Core:
-
Lactose monohydrate.
-
Cellulose microcrystalline.
-
Magnesium Stearate.
-
Sodium starch.
Tablet Coat:
-
Polyvinyl alcohol.
-
Macrogol 3350.
-
Titanium dioxide.
-
Talc.
-
Methacrylic acid – ethyl acrylate copolymer (1:1) type A.
-
Sodium hydrogen carbonate.
Absorption:
Almost 60 % of the orally administered Erlotinib is absorbed and reaches systemic circulation. The peak plasma concentration is attained within 4 hours. The presence of food increases the bioavailability to almost 100 %. Hence, administration on an empty stomach is recommended.
Distribution:
Approximately 93 % of Erlotinib binds to plasma albumin and alpha-1 acid glycoprotein (AAG). The apparent volume of distribution for Erlotinib is 232 liters.
Metabolism:
In vitro, Erlotinib is primarily metabolized by CYP3A4 and, to a lesser amount, by CYP1A2, as well as the extrahepatic isoform CYP1A1.
Excretion:
About 83 % of the orally taken Erlotinib is excreted in the feces and 8 % in the urine. The total body clearance is 5.3 L/hr for cancer patients, which is increased to almost 24 % in smokers.
The median half-life of Erlotinib for elimination is 36.2 hours. Thus, it would take 7-8 days to attain steady-state plasma levels.
Toxicity:
Erlotinib has not caused mutagenesis or impairment in fertility, as depicted from in vitro animal studies. However, toxicity may occur. The management of Erlotinib toxicity is as described:
Mild to Moderate Toxicity:
Treatment is symptomatic and supportive. Treat persistent nausea and vomiting with several antiemetics of different classes. Administer colony-stimulating factors (Filgrastim or Sargramostim) as these patients are at risk for severe neutropenia.
Severe Toxicity:
Supportive and symptomatic care is provided. These individuals risk developing severe neutropenia, thus providing them colony-stimulating agents (Filgrastim or Sargramostim). Patients with severe thrombocytopenia, anemia, or bleeding may require platelet and packed red blood cell transfusion. The treatment of severe nausea and vomiting may involve the use of several medications from several pharmacological classes.
Warning and Precaution:
-
Before receiving the prescription, it is important to communicate any prior history of allergies or hypersensitive reactions to any medications.
-
Rare reports of incidents similar to Interstitial Lung Disease (ILD), including fatalities, have been made. If sudden development of persistent, new, or unexplained respiratory symptoms, including dyspnea, coughing, or fever, develops, stop administering the medication.
-
Cases of renal insufficiency and acute renal failure, including fatalities, have been reported. In patients at risk for dehydration, monitor electrolytes, and renal function. Stop the medication in case of dehydration.
-
Hepatic failure and hepatorenal syndrome (including fatalities) have been reported. Follow up on routine liver function tests. If severe changes in liver function occur, discontinue the use of the drug.
-
There have been reports of severe gastrointestinal perforations. The drug is to be discontinued in this case.
-
Skin conditions with bullous and exfoliative symptoms, including mortality, have been observed. Discontinue use if these symptoms appear.
-
The administration is to be stopped if symptoms of corneal perforation and ulceration.
-
Fetal risk has been observed. Avoid prescribing during pregnancy.
-
Monitoring is required for patients on warfarin therapy.
Dosage Form:
-
Erlotinib is available in tablet form.
-
It is marketed as 25 mg, 100 mg, and 150 mg tablets. Always follow the dosage as prescribed by the physician. Never take the medication without a doctor's approval. Do not share prescriptions with others.
-
The tablet is round, white, and film coated with ‘T’ imprinted on its surface and dose (25, 100, 150 ) on the other surface.
Monitoring Considerations:
-
Metastatic Non-Small Cell Lung Cancer: Before starting, check plasma for EGFR exon 19 deletions or exon 21 (L858R) replacement mutations (if not detected in plasma, tumor tissue should be tested if available) has a companion diagnostic test authorized by the FDA (Food and Drug Administration)
-
Liver function tests: Periodically in all individuals, more often in those with biliary blockage or liver disease (total bilirubin greater than the ULN or Child-Pugh A, B, C)
-
Renal function: Monitoring is required, particularly in people who are at risk for dehydration periodically, especially in patients at risk of dehydration, check serum electrolytes.
Contraindications:
Erlotinib is contraindicated in patients with hypersensitivity reactions to the drug.
Clinical Trials:
1. Monotherapy As Maintenance Treatment for NSCLC: In a randomized, double-blind, placebo-controlled trial carried out in 26 countries on 889 patients with metastatic or locally advanced NSCLC whose disease did not progress during first-line platinum-based chemotherapy, the safety and efficacy of Erlotinib as maintenance treatment of NSCLC were demonstrated. Erlotinib 150 mg or placebo was given orally once daily to patients in a 1:1 randomization until disease progression or intolerable side effects.
Results: In patients with EGFR IHC-positive tumors, the progression-free survival (PFS) and overall survival ( OS) Hazard Ratios were 0.69 and 0.77, respectively. Patients with malignancies that tested negative for IHC had PFS and OS Hazard Ratios of 0.77 and 0.91, respectively.
2. Along With Other Chemotherapeutic Agents: The concomitant administration of Erlotinib with platinum-based chemotherapy [Carboplatin and Paclitaxel or Gemcitabine and Cisplatin] did not show any therapeutic effect in two multicenter, placebo-controlled, randomized studies including over 1000 patients with locally advanced or metastatic NSCLC.
3. Single Agent as Second-Line or Third-Line Therapy for NSCLC: In a randomized, double-blind, placebo-controlled trial, 731 patients with localized or metastatic NSCLC who had failed at least one chemotherapy regimen were evaluated for the effectiveness and safety of Erlotinib as a single-agent. Erlotinib 150 mg or placebo was administered orally once daily to patients in a 2:1 randomization until disease progression or intolerable toxicity.
Results: The Erlotinib group's median overall survival was 6.7 months, compared to 4.7 months in the placebo group.
Other specifications:
Erlotinib in Pregnant Women:
Use effective contraception while receiving therapy and for at least two weeks after finishing the final pill if you could become pregnant. Inform your doctor immediately if you become pregnant while using Erlotinib, and they will decide whether to continue the medication.
Erlotinib in Lactating Women:
Avoid breastfeeding while using Erlotinib for at least two weeks after finishing the last tablet. If Erlotinib is excreted in human milk is unknown. Given that many medications are excreted in human milk and that Erlotinib may produce major adverse effects in nursing infants, a choice should be made regarding whether to stop breastfeeding or stop the medication, taking into account the significance of the medication to the mother. Therefore, using this medication, see your doctor or pharmacist if the patient pregnant, nursing, suspect that the patient may be pregnant or are planning a pregnancy.
Erlotinib in Pediatric Patients:
The safety and efficacy of Erlotinib are not yet established in pediatric patients.
Erlotinib in Geriatric Patients:
Between patients 65 years of age and younger, there were no general differences in safety or efficacy.
Drug Interactions:
Drugs interact with food, beverages, supplements, or other drugs, which may result in unwanted side effects.
The common interactions of Erlotinib are as listed:
1. Other Drugs That May Have Interactions:
- Acenocoumarol.
- Amiodarone.
- Boceprevir.
- Carbamazepine.
- Cimetidine.
- Ciprofloxacin.
- Clarithromycin.
- Cobicistat.
- Conivaptan.
- Dexlansoprazole.
- Enzalutamide.
- Esomeprazole.
- Famotidine.
- Fosphenytoin.
- Idelalisib.
- Indinavir.
- Itraconazole.
- Ketoconazole.
- Lansoprazole.
- Lopinavir.
- Lumacaftor.
- Mitotane.
- Nefazodone.
- Nelfinavir.
- Nizatidine.
- Omeprazole.
- Pantoprazole.
- Phenobarbital.
- Phenprocoumon.
- Phenytoin.
- Posaconazole.
- Rabeprazole.
- Ranitidine.
- Rifabutin.
- Rifampin.
- Rifapentine.
- Ritonavir.
- Saquinavir.
- St John's Wort.
- Telaprevir.
- Telithromycin.
- Voriconazole.
- Warfarin.
2. With Alcohol: Alcohol beverages should be limited while taking Erlotinib as it may increase the risk of perforations in the stomach.
3. With Food: Avoid grapefruit or grapefruit juice while taking Erlotinib, as it may decrease the drug's effectiveness.












