Introduction:
The use of local anesthetics has continued to increase in clinical practice as there is increased interest in using regional techniques for surgery and treating chronic pain.
Anesthesia can be of two types:
-
Topical Anesthesia: Using topical anesthetics during minor operations can significantly reduce discomfort, agony, and anxiety.
-
Local Anesthesia: "local anesthesia" means a lack of sensation caused by a temporary blockage of nerve transmission at the application site.
They are available in various forms, such as gel, sprays, ointments, and patches. They are applied with a cotton tip applicator, blunted syringes, and aerosol containers with cannulas. Could be offered products in single-dose applicators or multidose containers. The single unit-dose applicators make the calculation dose more precise and help avoid cross-contamination.
What Are the Ideal Properties of an Anesthetic Drug?
-
When injected, a local anesthetic solution should not cause any irritation to the tissues.
-
It should not cause any allergic reactions.
-
Have a rapid onset and sufficient time.
-
Be completely reversible.
-
Have very little or low systemic toxicity.
-
Be selective to the nociceptive pathway (perception or sensation of pain).
What Is the Basic Structure and Pharmacology of Topical Anesthetics?
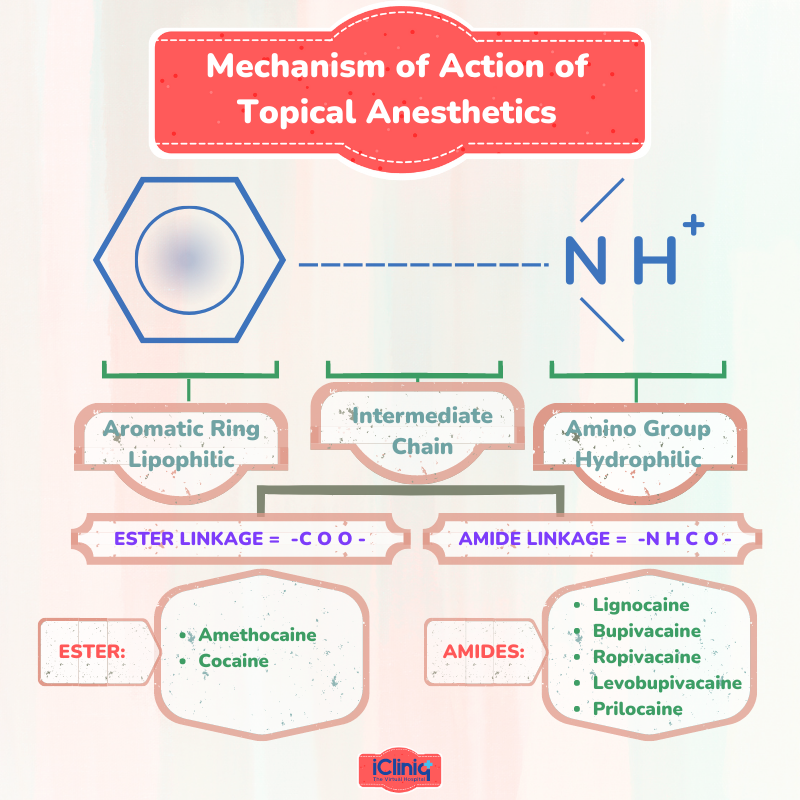
They are weak bases: they consist of an aromatic ring, an intermediate-length ester or amide bond, and a tertiary amine. The intrinsic characteristic of these drugs is essentially determined by the aromatic ring, which determines the lipid solubility that permits diffusion through the nerve cell membrane. The ability to attach to proteins depends on their amine and aromatic components.
What Are the Various Examples of Ester-Type Anesthetics?
-
Esters of Benzoic Acid: Butacaine, Cocaine, Ethyl aminobenzoate (Benzocaine), Hexylcaine, Piperocaine, Tetracaine.
-
Esters of Para-Aminobenzoic Acid: Chloroprocaine, Procaine, Propoxycaine.
What Is the Mechanism of Action of Topical Anesthetics?
Topical anesthetics reversibly block nerve conduction close to their application site, targeting free nerve terminals in the skin or mucosa, providing a temporary loss of sensation in the targeted region. Reducing the permeability of sodium ions into the nerve cell membranes, potentially due to competition with calcium-binding sites that regulate sodium permeability, prevents the conduction of nerve impulses. As a result, the altered permeability decreases depolarization and increases the excitability threshold until the ability to generate an action potential is lost.
What Is the Onset, Anesthetic Depth, and Duration of Action of Topical Anesthetic Drug?
The onset of action, depth of the anesthesia, and duration of action are based on the ionization constant (pKa), pH of the environment, lipid solubility, protein binding capacity, and vasodilatory effects of the anesthetic drug. Factors that have an additional influence are the site of application (onset is faster at mucosa and sites with thin stratum corneum), vascularity of the tissues in the applied area, the surface area, and duration of application.
For example, when the ionization constant (pKa) is high, the local anesthetic's onset and action are delayed. The more the protein binds, the longer the duration of action.
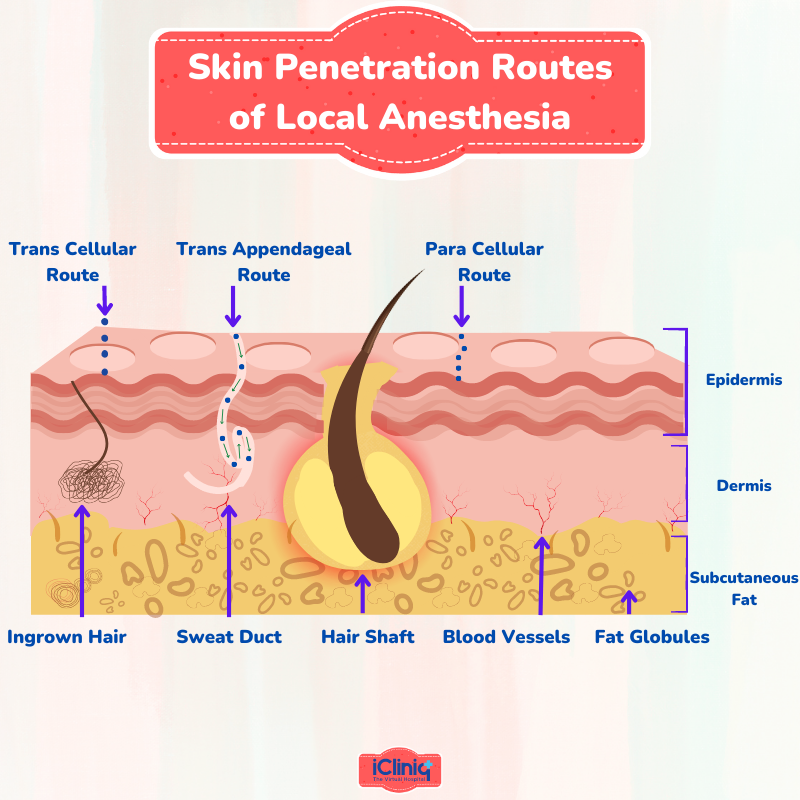
What Are the Skin Penetration Routes of Local Anesthesia?
There are three ways for a local anesthetic solution to cross the stratum corneum, which is a major barrier:
-
Intercellular route (through the intercellular spaces of the cornified keratinocytes).
-
Para or transcellular route (through the cornified cells).
-
Transappendageal route or shunt pathway (through the openings of the hair follicles and sweat glands).
How Is Ester-Type Topical Anesthetic Solution Metabolized?
Pseudocholinesterase hydrolyzes ester local anesthetic solutions in plasma. The faster the hydrolysis, the lesser the virulent potential. Chloroprocaine (least toxic) and Tetracaine (most toxic). These allergic reactions are due to para-aminobenzoic acid, a major metabolite.
How Are Ester Topical Anesthetics Excreted?
Kidneys are the primary excretory organs for the local anesthetic solution. The total dosage of local anesthetic drugs given to the patient during the procedure will be excreted in the urine unchanged. In the case of ester-type local anesthetics, small traces are found in urine because the local anesthetic drug is hydrolyzed in the plasma.
What Is the Maximum Dose of Administration of Anesthetics?
The total amount of the drug, whether it is administered with or without Epinephrine, the method employed, the rate of administration, and the tissue's vascularity should all be taken into account while administering local anesthetics.
Table Shows the Dosage of Ester-Type Local Anesthetic Drugs:

What Are the Allergic Reactions to Ester-Type Anesthetics?
-
Patients can be allergic to methylparaben (a bacteriostatic anti-fungal agent) or metabisulphite, a preservative in the anesthetic solution. Allergic reactions to esters are widespread.
-
Benzocaine, used as a topical anesthetic, can cause aphthous ulcers. After latex, Benzocaine is identified as one of the most allergenic substances in dental practice.
-
Allergy to local anesthesia is extremely rare, but such an incident is not completely impossible. Hence, the surgeon should know the signs and symptoms of allergic reactions.
-
A conscious patient suffering from an anaphylactic response would often have a combination of symptoms involving skin (rashes, hives, urticaria, erythema, mottling), respiratory (wheezing, dyspnea from the airway, and angioedema), and gastrointestinal systems (cramping, vomiting, diarrhea).
-
For an unconscious patient, the clinical features have been masked and present with cardiovascular collapse (hypotension or asystole) and compromise on the respiratory system, such as (hypoxia, dyspnea, tachypnea, coughing, and bronchospasm).
What Are the Indications of Ester-Type Topical Anesthetics?
-
In General: To reduce pain before injection and intravenous infusion lines access for the treatment of trigeminal neuralgia, to relieve itching and pain caused due to burns and skin eruptions.
-
In Ophthalmology: To perform Schirmer’s test, remove small foreign particles from the eye, ease procedures such as cryotherapy, biopsy, curettage of the molluscum contagiosum, and repair any lacerations.
-
In ENT: Topical anesthesia is used in the tympanic membrane for tympanocentesis, myringotomy, transtympanic injections, and for the placement, removal, or manipulation of the pressure equalizing tube. In the nasal cavity: during routine endoscopy procedures, nasal debridement, control of bleeding from the nose, treatment of fractures in the nose, and management of abscesses and hematomas.
-
In Dentistry: For the management of dry socket and aphthous ulcer, simple extraction of a primary tooth, placement of a rubber-dam clamp, surgical treatment of the mucosal surface, incision of the superficial submucosal abscess, drainage of the peritonsillar abscess, inhibition of gag reflexes during endotracheal intubation, routine dental radiographs, and impression making, control of pain in a wounded area, placement of orthodontic bands and also for routine scaling and root planing and to treat severe dentoalveolar fractures like maxillomandibular fixation for mandibular fractures.
Conclusion:
With continued research and innovation, the field of local anesthesia will continue to advance the eternal quest for pain control. It is the responsibility of the practitioner to select the safe drug and tailor the dose to be administered based on individual needs. Even though adverse reactions to the topical anesthetic are rare, medically compromised patients, children, and elderly patients have an increased risk.












