What Is Relapsing Polychondritis?
Relapsing polychondritis is a multi-system immune-mediated inflammatory disorder that can be detrimental and is characterized by recurrent episodes of acute inflammatory destruction of the cartilaginous tissues and other connective tissue organs of the body. The term “relapsing polychondritis” was coined in the year 1960 by Pearson et al.
The disease is often marked by repeated inflammatory episodes of chondroid tissues, mainly involving the cartilaginous structures of the ear, nose, peripheral joints, and the tracheobronchial tree, which result in progressive deterioration and destruction of the affected tissues and organs.
What Are the Other Synonyms of Relapsing Polychondritis?
-
Chronic atrophic polychondritis.
-
Systemic chondromalacia.
-
Relapsing perichondritis.
-
Von Meyenburg disease.
What Is the Frequency of Relapsing Polychondritis?
The incidence rate for the disease is estimated to be approximately 3.5/1,000,000/year. It most commonly occurs in the age group of fourth to fifth decades of life with a slight female predilection.
What Triggers Relapsing Polychondritis?
The cause of relapsing polychondritis is unknown. Researchers identified genetics, long-term stress, and a combination of various environmental factors as the main triggering factors for the initiation of the disease pathogenesis.
What Is the Pathogenesis of Relapsing Polychondritis?
Autoimmunity directed against specific chondroid tissues may play a pivotal role in the pathogenesis of relapsing polychondritis. Autoantibodies (antibodies that are directed against the individual’s own proteins) are directed against collagens II, IX, and XI circulating in the patient’s serum. Type II collagen is, therefore, the most important target for circulating autoantibodies.
What Are the Symptoms of Relapsing Polychondritis?
-
Chondritis and polyarthritis are the most common clinical manifestations of relapsing polychondritis. Chondritis is cartilage inflammation, and polyarthritis is the inflammation of joints.
-
Cataracts (cloudy lens).
-
Small blood vessel vasculitis.
-
Inflammation of the elastic cartilage of the external ear.
-
The onset is abrupt, with painful erythematous and edematous cartilaginous tissue of the ear with sudden onset.
-
The ear progressively loses its normal anatomy, appearing nodular or verrucous.
-
The cartilage of the nose may also be involved leading to a saddle nose.
-
Painful, reddish eyes.
-
Severe rib, throat, or neck ache.
-
Difficulty in swallowing food.
-
Difficulty in breathing.
-
Erythematous rashes.
-
Loss of weight.
-
High temperature.
-
Weakness and lethargy.
-
Tiredness.
-
Sweating at night.
-
Enlarged lymph nodes.
-
Chronic cough.
What Are the Other Diseases Associated With Relapsing Polychondritis?
The most common diseases associated with the disorder include
-
Cutaneous leukocytoclastic vasculitis (inflammation of the skin's small blood vessels of the dermis).
-
Systemic vasculitis with severe organ involvement (inflammation of the blood vessels in various organs).
-
Polyarteritis nodosa (a multi-system disorder characterized by damage of various blood vessels).
-
Wegener’s granulomatosis (a condition characterized by inflammation of the blood vessels of the nose, throat, ears, kidneys, and lungs).
-
Churg Strauss syndrome (a disorder characterized by inflammation of blood vessels).
-
Behcet’s disease (a disease-causing blood vessel inflammation throughout the body).
-
Systemic lupus erythematosus (an autoimmune inflammatory disease causing widespread organ damage).
-
Sjogren’s syndrome (a disorder characterized by dry eyes and dry mouth).
-
Hashimoto’s thyroiditis (an autoimmune disease that attacks the thyroid cells).
-
Systemic scleroderma (a condition that causes tightening of the skin).
-
Rheumatoid arthritis (an inflammatory disorder of the joints).
-
Myelodysplasia (a type of blood cancer where red blood cell production is disrupted).
-
Psoriasis (a skin disease that causes a rash with itchy and scaly patches).
-
Vitiligo (a condition causing loss of skin color in patches).
-
Reactive arthritis (swelling and joint pain triggered by an infection).
-
Ulcerative colitis (a disorder characterized by ulcers in the digestive tract).
-
Diabetes mellitus (a disease characterized by high blood glucose levels).
How Is Relapsing Polychondritis Diagnosed?
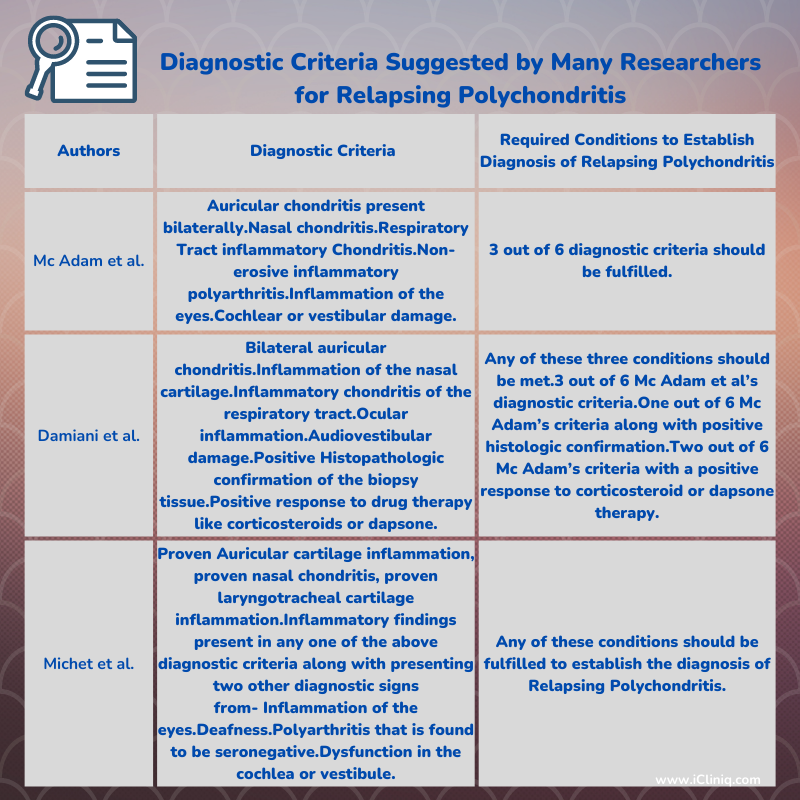
The diagnosis of relapsing polychondritis mainly relies on the patient’s clinical history, laboratory test findings, various imaging techniques, and histopathological examination after doing a biopsy of the inflamed site or organ. There is no specific blood laboratory test used to diagnose the disease. Many researchers for relapsing polychondritis suggest several diagnostic criteria:
What Are the Laboratory Findings for Relapsing Polychondritis?
-
Inflammatory Biomarkers- Patients suffering from acute episodes of relapsing polychondritis usually have elevated levels of inflammatory biomarkers, which include erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) that can be used to assess the disease severity and treatment response.
-
Cartilage-Specific Autoantibodies- They are usually present in the patient during acute recurring episodes of inflammatory polychondritis.
-
Other Antibodies- Antinuclear antibodies and antiphospholipid antibodies are other diagnostic tests that may be helpful for the evaluation and diagnosis of connective tissue diseases that are immune-mediated.
-
Rheumatoid Factor Test- This test measures the rheumatoid factors (proteins produced by the immune system that can attack healthy tissues of the body) in the patient’s blood.
What Are the Other Special Tests for Relapsing Polychondritis?
-
Imaging Techniques- Positron emission tomography scans, magnetic resonance imaging techniques, and computed tomography body scans are some imaging procedures that can be carried out to diagnose the disease.
-
Biopsy- Histopathological examination of the cartilaginous tissue demonstrates intense inflammation, tissue destruction, and chondritis which may be useful for diagnosing the disease.
-
Pulmonary Functional Tests- Pulmonary function tests that include inspiratory and expiratory volume measures also identify the extent of thoracic airway obstruction in relapsing polychondritis.
What Is the Treatment for Relapsing Polychondritis?
There is no guided specific treatment therapy for the management of relapsing polychondritis. Treatment is mainly symptomatic and directed at reducing the severity and progression of the disease. The mainstay of the treatment is to maintain the patency of the airways and stabilize the patient.
Administration of non-steroidal anti-inflammatory drugs, Corticosteroids, and Dapsone benefits some affected individuals. Drug therapy given for a longer duration does not halt the progression of the disease. Despite inclusive medical treatment, the prognosis is very poor in severely affected patients. Multiple new therapeutic approaches have been introduced successfully, such as tumor necrosis factor-alpha blockers (TNF-α blockers) in the management of patients who are treatment-resistant. Such biological markers also mitigate or even eliminate the process of disease severity and progression.
What Is the Diet Followed for Relapsing Polychondritis?
A low-fat, plant-based vegan diet devoid of animal proteins is called the McDougall Program and is recommended by many nutritionists to control the severity of the disease. It is easy to follow, and many patients are benefitted from the diet. The diet comprises no dairy or eggs. It aims at eliminating all kinds of meat with no added oils.
Conclusion
Relapsing polychondritis is a rare disorder with a life-threatening outcome. During the progression of the disease, multiple organs may be involved, and it is very difficult to establish the proper diagnosis. The therapeutic approach for treating the disease should be focused on the early detection of potentially destructing life-threatening conditions such as aortic aneurysms, defects in the heart valves, and narrowing of the respiratory tract airways. The various researchers' diagnostic criteria should be considered while diagnosing relapsing polychondritis.












