Introduction:
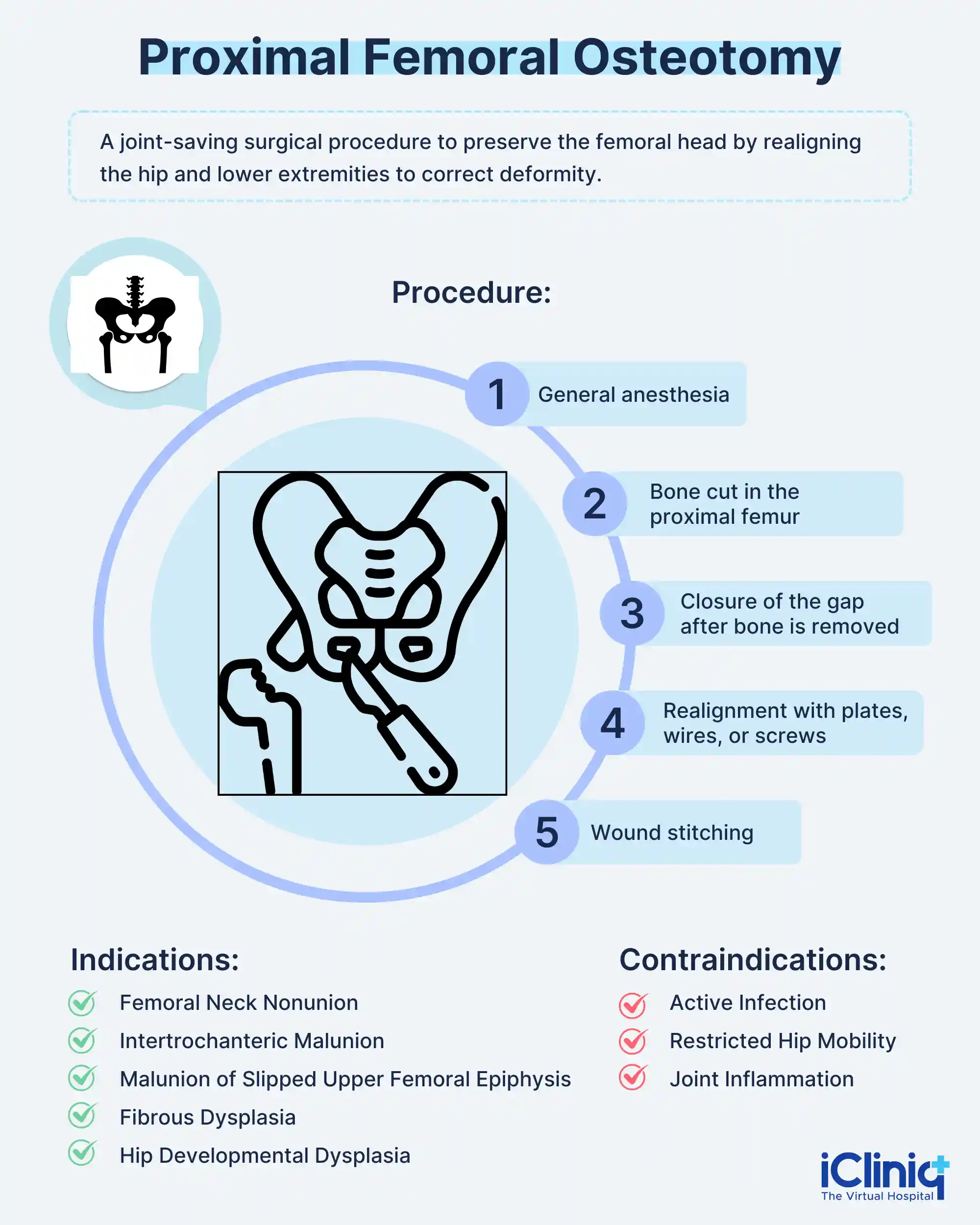
The preservation of the femoral head's biological integrity is essential to the joint-saving operation known as proximal femoral osteotomy. Proximal femoral osteotomies, once often carried out to treat hip dysplasia (the upper thigh bone's ball part is not completely covered by the hip socket) and hip arthritis (destruction of the hip joint's cartilage), are now less frequent. However, they are still employed in the management of congenital and acquired hip abnormalities, nonunions, and malunions of hip fractures. The purpose of proximal femoral osteotomy is to straighten the hip and lower extremities while also correcting the deformity.
Depending on where the osteotomy is made, proximal femoral osteotomies might be high cervical, intertrochanteric, greater trochanteric, or subtrochanteric.
What Are the Types of Proximal Femoral Osteotomy?
The following forms of proximal femoral osteotomies exist:
-
The Transposition Osteotomy: The distal fragment's longitudinal axis continues to be parallel to the proximal fragment's longitudinal terminal axis. Examples include Putti, Pauwel, and McMurray osteotomies.
-
The Angulation Osteotomy: The proximal fragment's longitudinal axis and the distal fragment's longitudinal axis are at an angle. For instance, adduction or abduction osteotomy (in the coronal plane) and extension osteotomy (in the sagittal plane) for fixed flexion deformity.
What Are the Indications and Contraindications for Proximal Femoral Osteotomy?
1. Indications: The following are some of the indications for proximal femur osteotomy.
-
Femoral Neck Nonunion: In the femoral neck nonunion, osteotomies are performed to change the fracture line's orientation from vertical to horizontal. This encourages osteogenesis (bone development) and fracture union by making the shear forces at the fracture site compressive.
-
Intertrochanteric Malunion: Varus (excessive inward angulation) is the consequence of an intertrochanteric fracture that has not healed. Varus angulation causes a Trendelenburg gait, a shortening of the ipsilateral (same side) femur, a shortening of the abductor muscles (a muscle that, when it contracts, pushes a body portion or limb away from the body's midline) or lever arm, and frequently a shortening of the trochanteric-pelvic abutment on abduction. Intertrochanteric osteotomy is used in these situations to realign the hip joint, bring back normal abductor mechanics, and correct the imbalance in leg length.
-
Malunion of Slipped Upper Femoral Epiphysis: A fracture malunion may develop if a dislocated slipped epiphysis heals in situ. This malunion is characterized by coxa vara (hip deformity), femoral (thigh bone) shortening, and femoral neck retroversion, with a considerable loss of hip mobility after remodeling. In circumstances where it is possible, osteotomies can contain the sphericity of the femoral head and straighten the slipping epiphysis. Osteotomies in cases that have healed are intended to rectify the varus, equalize limb length and abductor tension, and normalize gait.
-
Fibrous Dysplasia: Repeated microfractures of the femoral neck cause the femur to move and heal in a varus position, resulting in the well-known shepherd's crook deformity (hip deformity). The goal of a valgus-producing proximal femoral osteotomy is to restore a more normal relationship between the femoral head and the acetabulum while preventing the advancement of the deformity and the occurrence of a fracture.
-
Hip Developmental Dysplasia: Developmental hip dysplasia in adults causes both acetabular and femoral deformities. Femoral neck valgus and anteversion are present. The acetabulum is underdeveloped and shallow. Femoral head alignment is improved by a varus-producing proximal femoral osteotomy combined with derotation of the anteverted neck (the femoral neck tilts forward in relation to the rest of the femur).
2. Contraindications:
-
Active infection.
-
Hip mobility is restricted.
-
Inflammation in the joints.
Who Can Have a Proximal Femur Osteotomy?
A proximal femoral osteotomy may be right for patients if they:
-
Have a BMI under 30 and a healthy weight.
-
No more than 65 years of age.
-
Possess neither arthritis nor only mild arthritis.
-
Have undergone a failed complete hip replacement.
How Is the Patient Evaluated for Proximal Femoral Osteotomy?
1. Complete Clinical Evaluation:
-
Size of the malformation.
-
The deformation of planes.
-
The hips joint range of motion.
-
Any contracture of the hips or knees.
-
The difference in limb length.
-
Skin quality and previous incisions.
-
Any indications of the earlier infection.
2. Laboratory Tests:A complete blood count including ESR (erythrocyte sedimentation rate), CRP (C-reactive protein) are recommended before surgery to determine if there are abnormalities in the normal levels.
3. Imaging Tests:
-
Anteroposterior Standing Pelvic Radiography: This X-ray is advised to check the angle of the neck-shaft and hip joint sturdiness.
-
Lateral View: The X-ray view is recommended to rule out sagittal deviation.
-
MRI (Magnetic Resonance Imaging) and Computed Tomography (CT): These imaging studies are done to verify if there is a nonunion. And, also concerning osteomyelitis (an infection in the bone leading to swelling).
How Is Proximal Femoral Osteotomy Done?
For intraoperative fluoroscopic control, the patient is operated on a radiolucent fracture table. The method and location of the osteotomy would depend on the planned osteotomy and the osteotomy's underlying indication. For internal fixation, the lateral method is frequently employed. Typically, low intertrochanteric or subtrochanteric osteotomies are the only ones that require external fixation.
Procedure:
-
A general anesthetic will be provided while patients are lying on their backs.
-
The proximal femur, which is close to the hip joint, is cut.
-
An oscillating saw is used to cut the proximal femur.
-
The gluteus maximus and fascia lata muscles in the hip and thigh are similarly incised and retracted.
-
A predefined piece of the proximal femur is exposed and removed.
-
The doctor performing the surgery may choose to close the gap left after the bone is removed, either by grafting between them or by fusing the cut ends of the bones together.
-
The hip joint and proximal femur are then correctly aligned using metal plates, wires, and screws.
-
The wound is stitched up, and healing proceeds in a manner similar to how a fracture heals.
-
The procedure could take two to three hours.
What Are the Complications of Proximal Femoral Osteotomy?
The following are significant femoral osteotomy side effects:
-
Infection.
-
Neurological damage.
-
Nonunion.
-
Failure to achieve or maintain a complete correction.
-
Chronic discomfort following surgery.
-
Joint rigidity.
How Is the Recovery After Proximal Femoral Osteotomy?
-
Patients might need to stay in the hospital for one or two days following proximal femoral osteotomy surgery.
-
In order to lessen the need for and dosage of pain medications, the surgeon and the medical team will monitor the progress and establish a pain management strategy.
-
Patients will have to gradually start bearing weight.
-
Patients will be urged to stand with a walker on the second postoperative day and start touching down while bearing weight for longer durations of time.
-
For six to eight weeks, patients could need crutches to support their weight.
-
The majority of regular activities might not be able to resume for three months.
-
Getting back into athletics could take six to nine months.
Conclusion:
Results have been good when proximal femoral osteotomies are used to treat hip fracture nonunion and address congenital or acquired abnormalities. There are improvements in hip range of motion, gait, discomfort, leg-length inequality, and patient satisfaction. Long-term follow-up demonstrates that many patients who have proximal femoral osteotomies for osteoarthritis later develop the need for total hip arthroplasty.












