Introduction:
The specialization of thoracic anesthesia can be challenging. The anesthetist must meet the needs of creating lung isolation and the general difficulties faced during major surgery. One lung ventilation (OLV) and high intraoperative ventilatory pressures are risk factors for postoperative acute lung damage and hypoxemia, with an incidence of five to ten percent. Ventilator techniques have been designed to sustain oxygenation during OLV and postoperative lung injury. A crucial consideration in the anesthesia for general thoracic surgery is the choice of a lung separation device. A double-lumen endobronchial tube (DLT) is the commonest technique.
Left-sided DLTs are frequently employed to induce OLV in thoracic anesthesia. In contrast, right-sided positioning is technically more difficult due to the proximal take-off of the right upper lobe bronchus. One-lung ventilation can also be achieved with the help of bronchial blockers. One more challenging aspect for the thoracic anesthetist is the provision of analgesia for thoracotomy. Paravertebral block and thoracic epidural analgesia are used for post-thoracotomy pain relief.
The anesthesiologist and the surgeon struggle for the same organ during thoracic procedures, whether lung surgery or surgery requiring one-lung ventilation (OLV). Long-term impaired ventilation can have numerous implications beyond respiratory and hemodynamic physiology.
What Is the Preoperative Evaluation of the Patient?
Before surgery, every patient undergoing thoracic surgery must provide a detailed medical history and undergo a thorough physical examination. The assessment of patients before surgery to anesthesia is essential in lowering the complication rates for all types of anesthesia. Wheezing, rales, rhonchi, or other irregular breath sounds may indicate the need for additional medical treatment. The anesthetist should be attentive to any deviation of the trachea from the midline because of the difficulty in intubation or airway obstruction during anesthesia induction.
When a patient has chronic obstructive pulmonary disease, their electrocardiogram (ECG) may show signs of right atrial or ventricular hypertrophy. A larger P-wave indicates right atrial enlargement in the lead II. A low-voltage QRS complex causes lung hyperinflation. A forced expiratory volume in one second (FEV1) or forced vital capacity (FVC) of less than 70 percent of the anticipated value, or a ratio of FEV1 to FVC of less than 65 percent, is related to an elevated risk of pulmonary problems.
What Is a Spirometry Test?
Spirometry for patients undergoing lung resection, patients with unexplained dyspnea or pulmonary symptoms undergoing head and neck, orthopedic, or lower abdominal surgery, and patients with a history of smoking or dyspnea undergoing coronary bypass or upper abdominal surgery. Spirometric tests are often sufficient for forced vital capacity (FVC) and expiratory volume (FEV). FVC can be compared with normal values based on sex, height, and age and then expressed as a percentage of the predicted vital capacity (percent FCV) percent of FCV > 80 is normal, 70 to 80 percent is borderline normal, 60 to 70 percent show pulmonary disease, and less than 60 percent denotes significantly reduced pulmonary function.
FEV 1 is the volume of air that was forcibly exhaled in the first second of an FVC maneuver. Can compare FEV1 and FVC to distinguish between restrictive and obstructive lung disease (ratio FEV1/FVC = percent FEV1). The percent FEV1 is greater than 70 normally.
In Restrictive Disease: FEV1 and FVC decrease, so percent FEV1 remains normal.
In Obstructive Disease: FEV1 is reduced, so percent FEV1 is lowered.
A percent FEV1 below 70 indicates substantial airway resistance, making breathing harder under stress. An improvement of 15 percent in FEV1 following bronchodilator medication suggests that some airway blockage may be reversible in these individuals, and bronchodilators should be given preoperatively.
Patients not previously thought to be surgical candidates can now safely undergo a thoracostomy and video-assisted thoracoscopic surgery. Another method of determining the airway status is to monitor the flow-volume loop. After pulmonary resection, the quantity of functional lung tissue that will remain may be predicted through split-lung ventilation or perfusion tests, particularly helpful before pneumonectomy.
Radioactive xenon is injected intravenously, and radioactivity measured in each lung is equal to the regional perfusion. The inhalation of the radioactive gas assesses ventilation. The radioactivity measured in each lung equals the degree of regional ventilation. Following lung resection, decreased diffusing capacity is a reliable indicator of both pulmonary and cardiac problems, which is paramount to morbidity and mortality.
What Are the Factors Associated With Increased Risk for Thoracic Anesthesia?
Oxygen tension (PaO2) during pulmonary artery occlusion, carbon monoxide diffusion capacity, peak oxygen (O2) absorption, pulmonary artery occlusion, and exercise assessment before surgery. The patient's age influences the postoperative result, the operation's location and scope, the anesthetic's length, any pre-existing cardiovascular or neurological disorders, obesity, the anticipated level of postoperative discomfort, and the time between the operation and ambulation.
Table Shows the Cardiopulmonary Risk Index (CPRI) for Lung Resection:
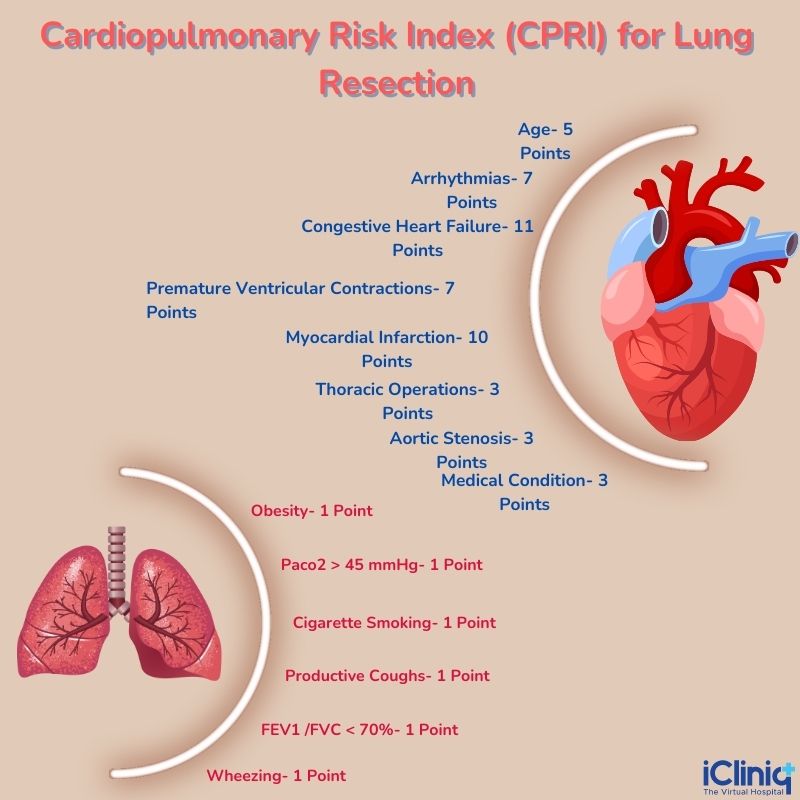
CPRI =CRI + PRI scores. A minimum CRI score of 3 is assigned to each patient because they are undergoing a thoracic operation. A CPRI score ≥ 4 was associated with a 22-fold increase in postoperative complications.
What Are the Risk Reduction Strategies?
Preoperative Risk Reduction Strategies Include:
- Encourage smokers to give up cigarettes for at least eight weeks.
- Patients with asthma or chronic obstructive lung disease should be treated for airflow obstruction.
- If a respiratory infection is present, treat it with antibiotics and postpone surgery.
- Start teaching patients about lung expansion techniques.
Intraoperative Risk Reduction Strategies Include:
-
Surgery should not go beyond three hours.
-
Administer spinal or epidural anesthesia.
-
Restrict the usage of pancuronium.
-
When feasible, do laparoscopic operations.
-
When feasible, substitute a less ambitious operation for upper abdominal or thoracic surgery.
Post-operative Risk Reduction Strategies Include:
-
Postoperative strategies include lung expansion maneuvers and pain control.
-
Use deep breathing exercises or spirometry incentives.
-
Use persistent positive pressure in the airways.
-
Utilize epidural anesthesia and block the intercostal nerves.
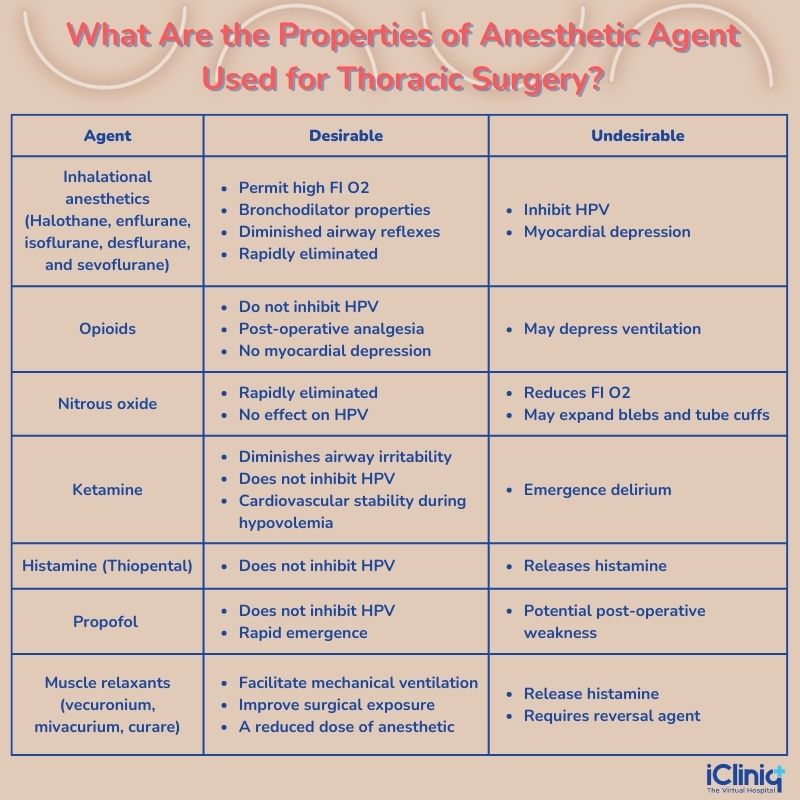
What Is the Choice of Anesthetic Agent?
Airway resistance is raised during general anesthesia by decreasing functional residual capacity (FRC). It is also increased during thoracic surgery by blockages caused by secretions or tumors, which might result from surgical insult, bleeding, and bronchospasm.
Chronic obstructive pulmonary disease, asthma, cystic fibrosis, and other lung diseases impact the capacity and reactivity of the airways and are linked with increased airway resistance.
What Are the Properties of Anesthetic Agent Used for Thoracic Surgery?
What Is Intraoperative Monitoring for Thoracic Surgery?
Noninvasive blood pressure, pulse oximetry, end-tidal capnography, ECG (electrocardiography), and temperature monitoring should be standard practice during thoracic procedures. A urinary catheter should be inserted before lengthy treatments and when epidural opioids are anticipated. Continuous oxygen and intra-arterial blood gas monitoring have an added advantage (CIABG) during thoracic surgery.
Conclusion:
The mortality rates have decreased due to novel advances in surgical techniques and anesthetic approaches in treating lung surgeries. Thoracic anesthetists should have expertise in managing the airway through ventilation procedures.












