What Is Arthritis?
Arthritis is a condition in which there is swelling and tenderness of one or more joints. It is more commonly seen in females than males. The common symptoms of arthritis may include pain and stiffness in the joints. The most common types of arthritis are osteoarthritis and rheumatoid arthritis.
The other types of arthritis are:
-
Ankylosing spondylitis.
-
Psoriatic arthritis.
-
Juvenile idiopathic arthritis.
-
Gout and calcium crystal diseases.
What Is Inflammatory Bowel Disease?
Inflammatory bowel disease (IBD) is the term used to describe two bowel conditions, namely Crohn's disease, and ulcerative colitis, marked by inflammation of the gastrointestinal (GI) tract. The digestive tract involves the mouth, esophagus, stomach, small intestine, and large intestine. Prolonged inflammation in the digestive tract can cause intestinal disorders like inflammatory bowel diseases.
What Are the Common Symptoms of IBD?
-
Fatigue.
-
Abdominal pain or cramping.
-
Bloody stools.
-
Low appetite.
-
Unintended weight loss.
The exact cause of IBD is unknown, but scientists believe that chronic inflammation might result from an immune system that does not work correctly. When triggered by an environmental factor, the immune system may become overactive and attack the GI tract by mistake.
Is There Any Link Between IBD and Arthritis?
IBD has been associated with arthritis through a genetic component or an inflamed gut. The common types of arthritis associated with IBD are psoriatic arthritis, ankylosing spondylitis, and reactive arthritis.
What Type of Arthritis Is Associated With IBD?
Two types of joint problems such as arthritis (with inflammation) and arthralgia (without inflammation), can occur in patients with inflammatory bowel disease (IBD). IBD-associated arthritis describes inflammatory arthritis associated with IBD like psoriatic arthritis, ankylosing spondylitis, and reactive arthritis. About 60 % to 70 % of the cases of arthritis seen in IBD patients are peripheral arthritis. The type of arthritis where large joints are affected is called oligoarthritis, indicating that fewer than five joints are affected.
About one to six percent of all inflammatory bowel disease patients may develop ankylosing spondylitis. It is a progressive inflammatory arthropathy that affects the sacroiliac joints and the spine. The joints that are commonly affected are the knees, elbows, wrists, hips, and ankles. Fusion of the spine may also occur in some cases.
Is Arthritis With IBD and Rheumatoid Arthritis the Same?
Arthritis that is associated with IBD is not the same as rheumatoid arthritis. Antibodies usually found in the blood of people with rheumatoid arthritis are not typically present in people with arthritis associated with IBD. People with rheumatoid arthritis will have an erosive and deforming arthropathy that will slowly destroy the joints requiring joint replacement surgery. In contrast, people with arthritis associated with IBD will not experience any erosive or deforming and there will not be any long-term damage to the joints.
What Are the Symptoms of Arthritis With IBD?
The symptoms of IBD may include,
-
Bloody diarrhea.
-
Crampy abdominal pain.
People having arthritis associated with IBD will have pain, swelling, and stiffness (especially in the morning) in those joints that are inflamed. The joint symptoms may often come along with the bowel symptoms. Therefore, there will be pain and swelling in the joints when the gastrointestinal symptoms become worse.
Common complaints may include:
-
Low back pain that is worse in the morning and better on movement.
-
A limited joint motion may develop more stiffness.
How Will You Diagnose Arthritis With IBD?
No test can confirm the diagnosis of arthritis associated with inflammatory bowel disease. Your doctor will ask about your medical history, especially whether you have inflammatory bowel disease. They will look for typical symptoms and will examine for inflamed joints.
-
Careful examination of the joints for swelling, limited motion, and tenderness is the best way to diagnose IBD arthritis.
-
X-rays of the involved joints can also be taken.
-
Laboratory testing is not an appropriate test for diagnosing IBD arthritis because it is usually associated with elevations in the value of inflammatory markers, which can also be seen in several inflammatory conditions.
-
Crohn's disease can be diagnosed by checking for the antibodies caused by a yeast called Saccharomyces cerevisiae, and ulcerative colitis can be detected by finding the anti-neutrophil cytoplasmic antibodies (ANCA) in the blood test.
-
Endoscopy can be done to detect the abnormality in the gut.
Which Drug Should Be Avoided in Patients With Arthritis-Associated IBD?
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the leading group of drugs that should be avoided in patients with IBD. Evidence suggests that these drugs can trigger flare-ups of the underlying IBD, so NSAIDs should not be recommended to treat arthritis if a patient's IBD is active. If a patient has quiescent IBD and the joint pain is very troublesome, clinicians can cautiously try an NSAID; in this situation, clinicians must inform patients of the risk that the drug will upset the gut.
What Therapies Can Be Done for Arthritis With IBD?
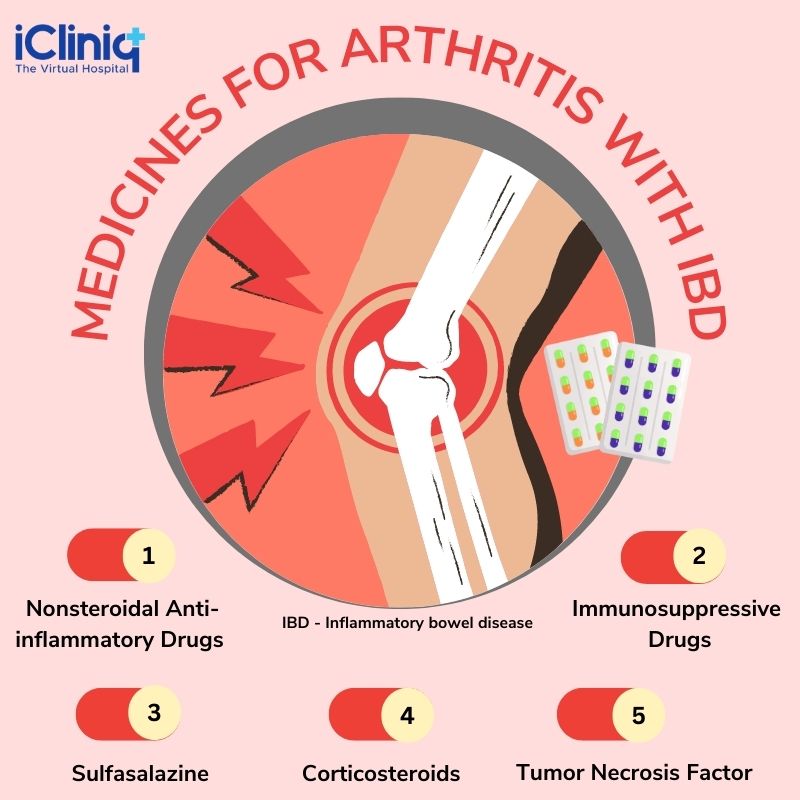
The treatment for IBD arthritis usually depends on the severity of the involved joint. Many therapies that are used to treat bowel disease will also treat joint problems. The medicines used to treat IBD arthritis include:
1) Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These are usually used in the treatment of IBD arthritis. But the problem is that these agents can aggravate gut inflammation and lead to stomach ulcers. However, newer NSAIDs like COX-2 selective inhibitors can reduce the risk of stomach ulcers.
2) Immune Suppressing Drugs: Methotrexate (MTX) and Azathioprine (AZA), a derivative of immunosuppressive medications, can be used in a few patients with IBD arthritis.
3) Sulfasalazine (SSZ): Sulfasalazine is a drug that can treat inflammatory bowel disease and joint inflammation in these patients with IBD arthritis who do not respond to NSAIDs. The common side effects associated with this drug are nausea, abdominal discomfort, and allergic reactions. It is a slow-acting drug that often takes about two to three months. A drop in the level of white blood cells and elevation in the level of liver enzymes can rarely occur while taking SSZ, which has to be monitored.
4) Corticosteroids: Corticosteroids like Prednisone can treat flaring of IBD, but they do not treat arthritis effectively. Steroid drugs can be directly injected into the inflamed joints to relieve the acute symptoms of arthritis.
5) Tumor Necrosis Factor (TNF): TNF antagonists have represented a significant advance in treating spondyloarthropathies and IBD. However, these cannot be given to every patient with IBD arthritis and can only be given in cases where there is a severe or resistant disease. These drugs can block the effects of TNF, a protein that is involved in inflammation in various parts of the body. Therefore, they appear helpful in treating IBD arthritis and rheumatoid arthritis.
The TNF antagonist drugs currently in use may include Etanercept, Infliximab, and Adalimumab.
Since TNF antagonists suppress the immune system, infections must be observed while administering these drugs. The other side effects may include:
-
Infusion reactions.
-
Injection site reactions.
-
Worsening of heart function in patients with heart failure.
-
Worsening of disease in patients with multiple sclerosis.
Conclusion
With treatment, the prognosis for IBD arthritis is usually good, although the condition is quite variable. Severe cases may develop significant joint damage and need surgery within a year or two, while other cases are considerably milder. Therefore, consult with your physician if you have symptoms of IBD like chronic diarrhea, crampy abdominal pain, unintentional weight loss, recurring fever along with signs of arthritis, like joint pain, swelling, or limited motion.












