What Is Hemophilic Arthropathy?
Hemophilia is characterized by a propensity to bleed as a result of inadequate clotting factors. Soft-tissue and intramuscular bleeding are two skeletal symptoms that may result from these conditions. The hemophiliac disorders that are most frequently linked to bone and joint issues are hemophilia A (factor XIII deficit) and hemophilia B or Christmas disease (factor IX deficiency). Both of these X-linked disorders only affect men because of the gene's recessive nature, while women may be carriers. The deficiency of clotting factors VII and IX causes hemophilia A and B, respectively.
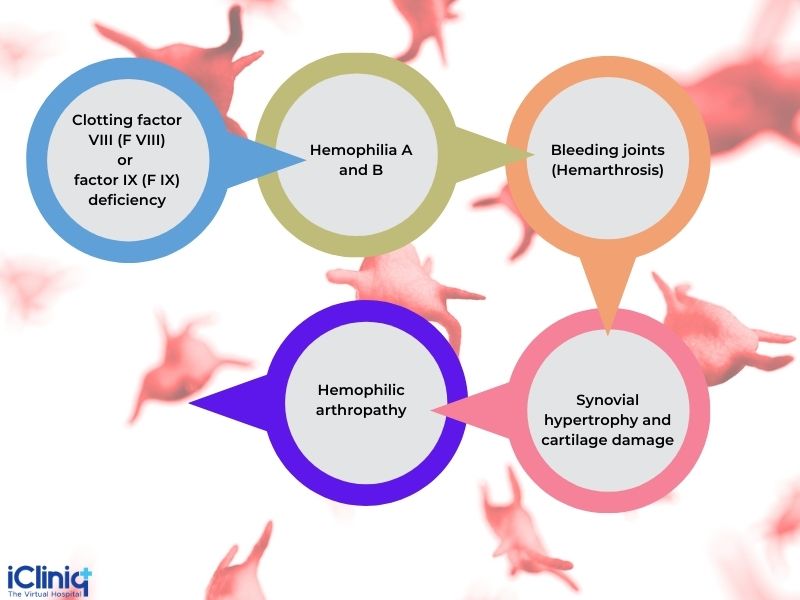
Severe hemophilia leads to hemarthrosis, which in turn leads to synovial hypertrophy and cartilage damage resulting in hemophilic arthropathy.
Recurrent bleeding into joints causes hemophilic arthropathy, which most usually affects the knees, elbows, and ankles. The release of damaging enzymes and an inflammatory reaction by the synovium are brought on by blood components in the joint. Joint damage may also result from hemorrhaging from the inflamed synovium itself.
Acute hemarthrosis may initially entirely disappear with treatment that involves giving the right clotting factor. Recurrent bleeding makes a full recovery impossible and causes muscular atrophy, contractures, and restricted joint motion. The radiographic alterations at this point are visible.
Who Is Affected by This Condition?
50% of hemophilia patients suffer from arthropathy. This condition occurs predominantly in males between 3 to 15 years.
Which Joint Is Most Affected by Hemophilic Arthropathy?

-
It can be monoarticular or oligoarticular.
-
Mostly affects the larger joints that are at increased risk of trauma.
-
This condition most commonly affects the knee.
-
Followed by elbow, ankle, shoulder, and spine.
What Are the Various Stages of Hemophilic Arthropathy?
Acute Hemarthrosis:
-
Replacement therapy and rehabilitation.
-
No clinically detectable consequences after treatment.
Subacute Hemarthrosis:
-
This happens after a series of hemarthrosis episodes in the same joint.
-
The joint and surrounding soft tissues do not entirely recover at this point.
-
Clinical symptoms continue and can be detected between bleeding episodes.
Chronic Arthropathy:
-
Symptoms include a considerable loss of muscular function and muscle-tendon contractures
-
Followed by frequent bleeding events in joints.
Paresthesias:
-
Iliacus hematoma compressing the femoral nerve causes paresthesias in the L4 distribution.
What Is the Pathophysiology of Hemophilic Arthropathy?
Hemophilic arthropathy, a crippling condition that has a serious effect on functionality and quality of life, is caused by frequent hemarthrosis and spontaneous joint hemorrhage. Early injuries and molecular alterations determine whether a chronic inflammatory condition will persist. Iron, cytokines, and angiogenic growth factors are crucial in the initiation of the inflammatory process that affects the synovial tissue, articular cartilage, and subchondral bone. One of the first effects of hemarthrosis is synovitis, which is associated with a high degree of neo-angiogenesis with resultant bleeding, synovial hypertrophy, and migration of inflammatory cells. It is still unclear how blood in the joint cavity damages the articular cartilage and subchondral bone, as well as the pathological mechanisms and molecular pathways involved.
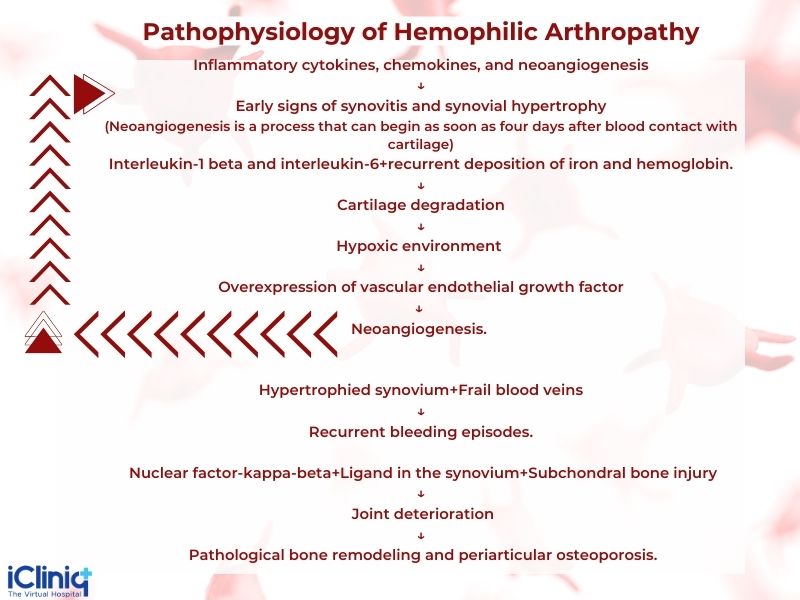
Chondrocyte apoptosis can be brought on by cytokines, matrix metalloproteinases, and hydroxyl radicals. The molecular triad of osteoprotegerin (OPG), receptor activator of nuclear factor b (RANK), and RANK ligand (RANKL) appears to play a significant role in the inflammatory process and is a member of the tumor necrosis factor receptor superfamily. As a result of the interactions between these pathogenic processes, hemophilic arthropathy, which is characterized by a fibrotic joint, develops.
How Do You Classify Hemophilic Arthropathy?
Classification is done based on Arnold-Hilgartner staging:
Stage 1: Soft tissue swelling.
Stage 2: Osteoporotic changes.
Stage 3: Subchondral cyst development. Grossly intact joint.
Stage 4: Cartilage loss with narrowing of joint
Stage 5: Severe arthritis of the affected joint.
How Is Hemophilic Arthropathy Diagnosed Clinically?
-
Periodic check-ups
-
Kids - once in six months.
-
Adults - once a year.
-
-
Clinical scores such as the Gilbert score and Hemophilia joint health score (HJHS).
What Is a Gilbert Score?
-
The Gilbert score is an additive score to measure joint problems.
-
Joint pain, hemorrhage, frontal plane deformation, presence of flexion contracture, range of motion (ROM) limitation, instability, muscle atrophy, presence of crepitus on motion, and joint edema are all factors that go into the Gilbert score.
-
The Gilbert score is used in clinical practice to evaluate patients with obvious arthropathy indicators.
What Is Hemophilia Joint Health Score?
-
HJHS is used to assess joint health in pediatric patients.
-
It can also be used to assess adults.
-
More sensitive to early changes of arthropathy.
What Are the Other Ways to Diagnose Hemophilic Arthropathy?
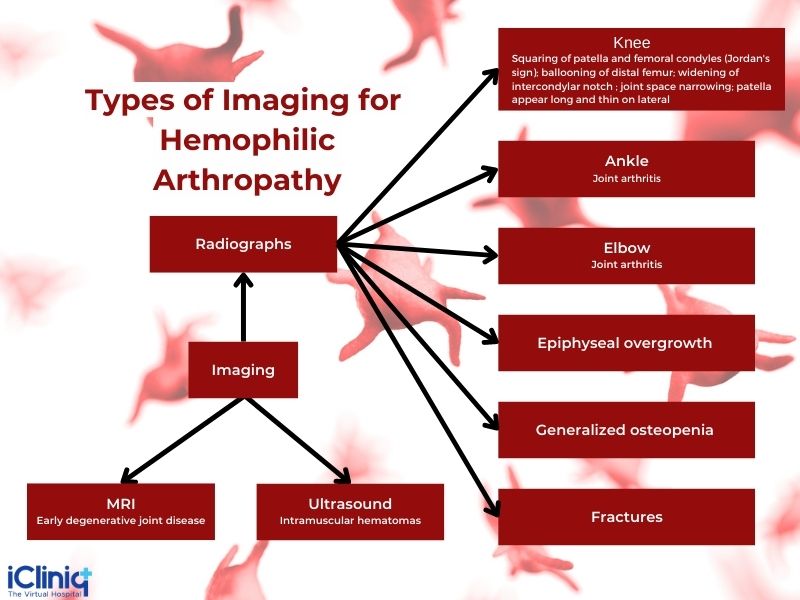
It can be diagnosed with imaging and laboratory tests.
-
Laboratory Tests: Screening for factor VIII inhibitors (including IgG antibodies).
-
Histology: Hypertrophy and hyperplastic changes to the synovium.
How Do You Manage Hemophilic Arthropathy?
Non-surgical Methods:
-
Compressive dressings are done in the affected area.
-
Steroids are given to help reduce inflammation.
-
Analgesics for pain relief.
-
Splints and braces - Immobilization.
-
Physical therapy to prevent contracture development.
-
Rehabilitation.
The administration of clotting factors is based on the stage of hemophilic arthropathy. It is given as home transfusion therapy to reduce the severity of arthropathies. Desmopressin is given for mild to moderate hemophilia A.
Surgical Methods:
-
Synovectomy - To prevent recurrence and decrease pain and swelling.
-
Synoviorthesis - Chronic hemophilic synovitis.
-
Total Joint Arthroplasties - End-stage arthropathy.
-
Arthrodesis - Arthropathy of the ankle.
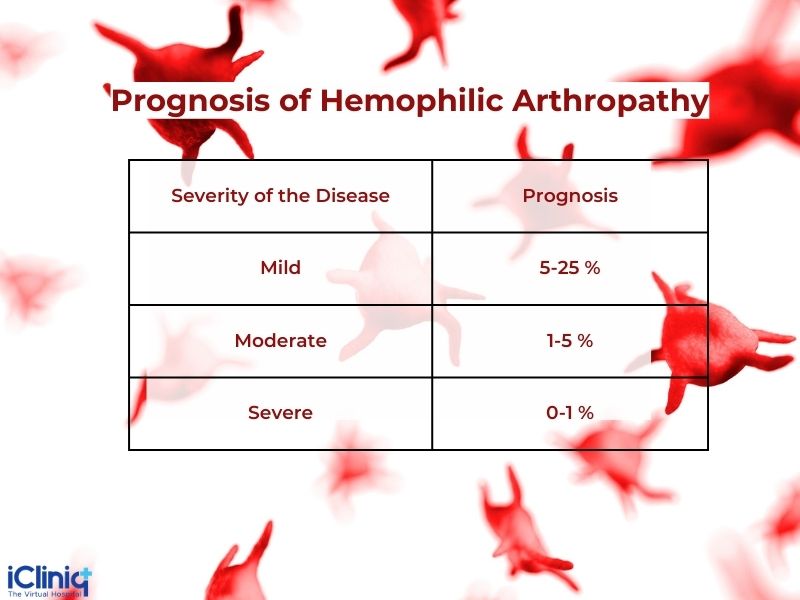
How Is the Prognosis of Hemophilic Arthropathy?
The amount of clotting factor deficiency ⇌ Severity of the disease ⇌ Prognosis
Conclusion:
In summary, an incapacitating disorder known as hemophilic arthropathy causes joint damage, persistent discomfort, and a poor quality of life. Recent research suggests that angiogenesis and intra-articular inflammation may play key roles in the pathogenic loop of hemophilic arthropathy. Joint bleeding promotes hemoglobin's release of iron, which triggers a chronic inflammatory process driven by cytokines and pro-angiogenic factors and, in turn, causes synovial pannus to expand and articular cartilage to deteriorate over time. It is interesting to note that there is a strong correlation between the types of gene mutation and the clinical phenotypes of hemophilia. Actually, it appears that either hemophilia A or hemophilia B patients' "null" mutations and/or missense mutations may considerably impact the severity of hemophilic arthropathy.












