Introduction:
A link between the bones of the body is called the joint. The joints form the network of the skeletal system and help with different types of body movements. The articulation between the bones at the joint is stabilized by various muscles, ligaments, and tendons.
Joints are classified according to their shape, structure, anatomy, function, and biomechanics. There are 360 joints in the adult human body. Most of the joints are mobile, allowing the bones to move, but few joints show only slight or no mobility.
What Is Arthropathy?
Arthropathy is a term to describe any disease of the joint. Arthropathy is a common cause of dysfunction and includes a prevalent combination of multiple chronic conditions. More than 350 million people in the world suffer from some kind of arthropathy which are the leading cause of work disability. It is more prevalent in older people aged 65 and above with a marked female predilection.
What Are the Causes of Arthropathy?
Arthropathies can be associated with infection, inflammation, accumulation of ionic crystals, a blood disorder, degenerative (age-related wear and tear), and debilitating diseases. Depending upon the cause, arthropathies are named as follows,
-
Reactive Arthropathy: Inflammatory response to infection from another part of the body. It commonly affects individuals between 20 to 40 years of age. Initially, this condition was known as Reiter’s syndrome.
-
Enteropathic Arthropathy: Acute reaction associated with the gastrointestinal inflammatory response. Usually, the large intestine (large bowel) is affected.
-
Crystal Arthropathy: Accumulation of tiny crystals in one or more joints.
-
Diabetic Arthropathy: Secondary changes in the joints caused by diabetes mellitus.
-
Neuropathic Arthropathy: Degeneration of the weight-bearing joint that may progress quickly. This condition often continues with ulcers, superinfections, and loss of functions and can result in permanent joint deformity.
-
Spondylarthropathy: Joint disease of the spinal bone. A pair of small joints in between the vertebrae (backbone) behind the spine are called facet joints. These joints may undergo degenerative changes and are named facet arthropathy.
-
Osteo Pulmonary Arthropathy: Joint dysfunction characterized by the enlargement at the ends of the long bones and clubbing (changes in the nails) in the fingers and the toes secondary to heart or lung disease.
What Are the Signs and Symptoms of Arthropathy?
Signs and symptoms of arthropathy differ based on the location of the disease and its specific features. But some of the common symptoms are:
-
Pain and tenderness in the joint region.
-
Mild swelling may be present with warmth and redness.
-
Loss of mobility and increased stiffness in the affected joint.
-
Fluid collection and retention.
-
Abnormal presence of air or gas in the joint tissues.
-
Destruction of bone and loss of bone mass.
-
Other secondary changes like muscle pain, fatigue, weakness, poor sleep, and decreased fitness.
What Are the Conditions That Fall Under Arthropathy?
Joint diseases can be classified as follows,
-
Arthritis:
Arthritis is the most common form of arthropathy that involves the inflammation of the joint. It is most common in elderly people. Arthritis can be primary or secondary to some other main disease. The most common form of primary arthritis is osteoarthritis or rheumatoid arthritis. The knee is the joint frequently affected by arthritis. In addition, the hip, hand, wrist, and spine can be involved.
-
Hemarthrosis:
Hemarthrosis is a blood disorder of the joint. It is associated with bleeding in the joint spaces caused by injury and is common in patients suffering from hemophilia (a disorder in which blood will not clot normally).
-
Crystal Arthropathy:
Gout and chondrocalcinosis are joint disorders classified under crystal arthropathy. Gout is characterized by the accumulation of uric acid crystals, and chondrocalcinosis is characterized by the accumulation of calcium pyrophosphate crystals. Thyroid disorders, kidney dysfunction, tissue damage, and being overweight are the risk factors associated with crystal arthropathy.
-
Joint Dislocation:
A joint dislocation is caused when the bones of the joint are displaced from its articular surface. It can happen after a sudden trauma. Some dislocations can be acquired through birth defects.
-
Synovitis:
Some joints have a special connective tissue that lines the articular surface of the joint called the synovial membrane. Synovitis is the inflammation of the synovial membrane and is often associated with arthritis. Sometimes a synovial cyst (fluid-filled sac) may develop in the joint, usually due to aging.
How to Diagnose Arthropathy?
Diagnosis can be made with a combination of investigations. They are,
-
Medical History:
The history of injury, birth defect, previous surgery, family disease, childhood disease, and allergy conditions are assessed.
-
Physical Examination:
The joint movements are examined by physicians by stretching and bending the joints. The next step is assessing the onset of the disease, the number of joints involved, symmetry, distribution, and pattern.
-
Blood Test:
The blood test is especially useful in the diagnosis of rheumatoid arthritis, which may indicate the presence of an anti-inflammatory process in the body.
-
Medical Imaging:
X-rays, CT (computed tomography) scans, MRI (magnetic resonance imaging), and a bone scan detect joint disease.
How to Treat Arthropathy?
-
Medications:
Painkillers and anti-inflammatory drugs are used to reduce pain and swelling. Steroids are used in auto-immune joint disorders.
-
Physical Therapy:
Stiffness and loss of movement in the joint are the main problems for patients with joint diseases. The main aim of physiotherapy is to increase the flexibility of the joint and aid in free movements.
-
Surgery:
Open or arthroscopic (minimally invasive) surgery is recommended for joint diseases.
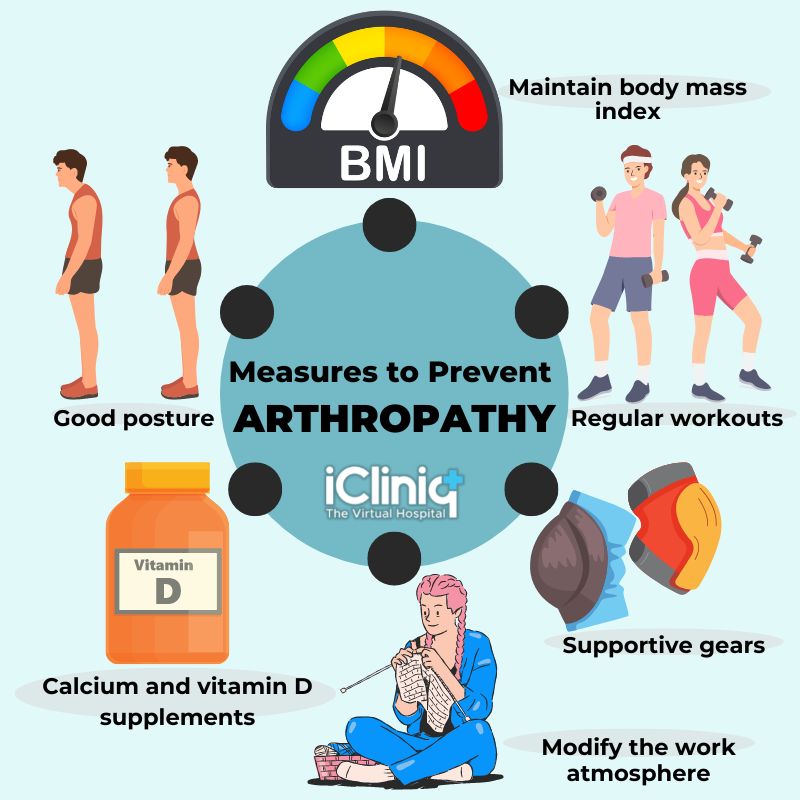
How to Prevent Arthropathy?
Arthropathy is usually an age-related debilitating disease.The following are certain measures that can prevent arthropathy or halt the disease progression.
-
Maintain body mass index.
-
Regular workouts.
-
Supportive gears like knee pads, elbow pads, protective shoes, and soles during sports activity prevent injury or strain over the joints.
-
Modify the work atmosphere or activity that can induce arthropathy.
-
Calcium and vitamin D supplements will maintain bone health, especially for post-menopausal women and the elderly.
-
Maintain good posture.
Conclusion:
Arthropathy is a broad and complex topic with many types, subtypes, and variations. Arthropathy is also associated with systemic effects, and some joint diseases do not have any cure and can severely diminish the quality of life. Therefore arthropathy is a major cause of serious disability in many people. However, in recent times, proper patient education, support programs, and current advanced treatment strategies give the hope of leading an active and productive life for patients suffering from arthropathies.













