Introduction:
The central nervous system comprises the brain and the spinal cord. It is the principal regulatory center responsible for conducting entire body functions. The central nervous system consists of two types of cells, neurons, and glial cells. Neurons act as messengers, and their prime function is to transmit messages in the form of an impulse from the brain to the entire nervous system and vice-versa. In contrast, the glial cells function to protect the neurons. In addition, they provide structural support and essential nutrients that are required by the neurons. The glial cells are of four types, and they are described below:
-
Microglia: Microglia act as scavengers by removing dead and degraded cells, thereby protecting the brain.
-
Astrocytes: Astrocytes are specialized star-shaped cells that are more in number than neurons by almost five times. They provide the neurons with structural support and essential nutrients. They also prevent the entry of toxic substances into the brain by forming a blood-brain barrier.
-
Oligodendrocytes: Oligodendrocytes form a protective myelin sheath around the nerves.
-
Ependymal Cells: These cells are responsible for forming cerebrospinal fluid, which shields the brain and the spinal cord.
Thus the glial cells are as important as neurons in maintaining the integrity of the central nervous system.
What Is Astrocytoma?
Abnormal growth or mass of cells is known as a tumor. Tumors can occur in any part of the body, and one occurring in the brain is a brain tumor. They can be benign (non-cancerous) or malignant (cancer). However, considering its location, a benign brain tumor can also be potentially fatal. As they grow, these tumors can compress the adjacent neurovascular structures or develop increased pressure in the brain, both of which can hinder the functions of the brain and cause fatal consequences.
Glial tumors account for over 60 % of tumors in the brain, and the most common among them is astrocytoma. Astrocytomas are brain tumors originating from the glial cells astrocytes. They are potentially considered low-grade malignancies due to their high chance for recurrence, and progressively they can turn into high-grade malignant tumors. They are more common in adult males than females. They mainly occur at the apex or the top of the brain though some may occur at the base or in the spinal cord. The symptoms depend on the location of the tumor. Headaches, seizures, and nausea are the most common symptoms associated with astrocytoma of the brain. Spinal astrocytoma may cause weakness or paresthesia of the limbs, bowel and bladder dysfunction, and difficulty walking. The prognosis entirely depends on the grade of astrocytoma, which is given by the World Health Organization (WHO).
What Are the Types of Astrocytoma?
According to WHO, astrocytomas can be classified into four grades. They are mentioned below:
-
Grade I: It is the most benign form of astrocytoma. It is non-cancerous, and it does not spread to any other parts. It usually occurs in children. It is also called pilocytic astrocytoma.
-
Grade II: It is also known as diffuse astrocytoma. It is slow-growing, yet it tends to invade adjacent structures.
-
Grade III: It is known as anaplastic astrocytoma. It is a malignant tumor and is primarily seen in adults.
-
Grade IV: It is known as glioblastoma and is one of the most aggressive types of cancer. It is the most common form of astrocytoma. It can present as a primary tumor or a grade I can progress into glioblastoma. It causes extensive brain damage and advances swiftly.
What Are the Causes of Astrocytoma?
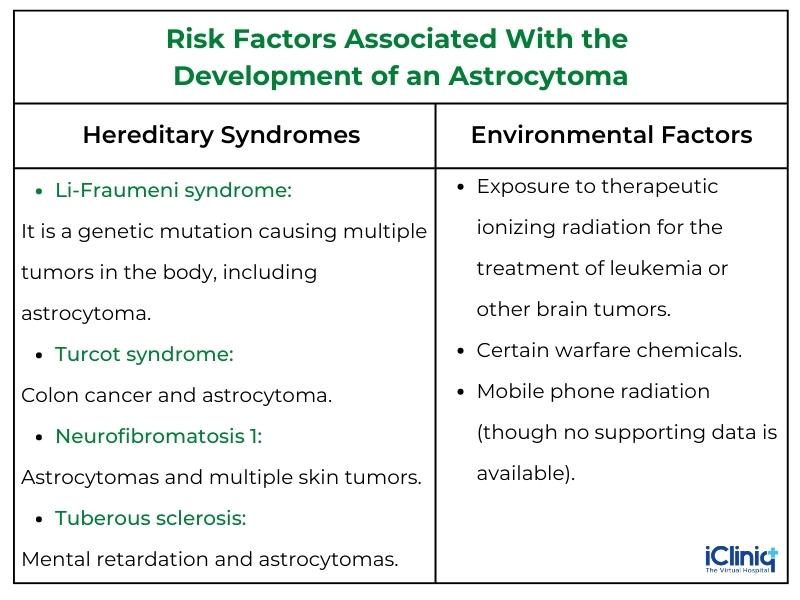
Astrocytomas are considered sporadic tumors as a definitive etiological factor that cannot be localized. However, there are certain risk factors associated with the development of an astrocytoma which are enlisted below:
What Are the Symptoms of Astrocytoma?
The symptoms of astrocytoma depend on the size and location of the tumors. Early symptoms include:
-
Constant headaches.
-
Vomiting.
-
Blurred vision.
-
Loss of memory.
-
Altered behavior.
-
Fatigue.
-
Weakness or numbness of the limbs.
-
Altered speech.
What Is the Role of Imaging Modalities in the Diagnosis of Astrocytoma?
Diagnosing astrocytomas can be challenging because of the overlapping symptoms with other neurological conditions occurring in the same location. However, an exhaustive clinical examination, detailed physical history, and diagnostic tests cumulatively can lead to the diagnosis of astrocytoma. Various neuroimaging techniques used in diagnosing astrocytoma are described below:
1. Radiography: A conventional x-ray is of limited value in diagnosing astrocytoma. The findings may be nonspecific. However, radiographs may prove beneficial in assessing spinal changes, such as spinal curvature and spinal instability, that may occur postoperatively.
2. Computed Tomography (CT): CT offers limited diagnostic value in assessing spinal tumors. The bony changes may be observed with a conventional CT; however, they are late secondary findings of astrocytoma. CT myelography may prove beneficial in patients in whom MRI is contraindicated. Myelography is an invasive diagnostic procedure that is considered the gold standard for diagnosing spinal cord abnormalities. They can precisely image the spinal column, nerve roots, spinal cord, and meninges. A contrast material is injected into the spinal column and imaged using CT. Any spinal cord tumor usually appears in a CT myelogram as a cord expansion.
3. Ultrasonography: Intraoperative ultrasound can aid in determining the extent of the lesion, tumor margin, and any associated cysts that need to be drained before surgical resection.
4. Magnetic Resonance Imaging (MRI): MRI is the first choice in diagnosing spinal cord tumors. Its excellent image resolution and precision make it an excellent neuroimaging tool. On MRI, a spinal tumor can be classified into three types:
-
Extradural: These tumors arise from the vertebral bodies.
-
Intradural: They arise from the meninges, the dura mater (the outermost protective covering of the spinal column), or the nerve root.
-
Intramedullary: They originate from the spinal cord; astrocytomas are intramedullary tumors.
Enlargement of the spinal cord is prominent at the site of the tumor. This feature may help differentiate a tumor from an inflammatory or non-neoplastic condition. Contrast MRIs are more specific. They can help differentiate a low-grade tumor from a high grade. When the tumor takes up the contrast, they appear bright on the image and are considered high-grade astrocytoma. In contrast, low-grade tumors do not take up much of the contrast material.
-
MRI Spectroscopy: This procedure works by determining the presence of certain chemicals in the brain. It is non-invasive but not very specific. A normal brain is rich in a chemical known as NAA (N-acetyl aspartate). Whereas the presence of a tumor will demonstrate a significant amount of a chemical known as choline. Hence the abundance of choline in spectroscopy should raise the suspicion of a tumor.
- Functional MRI (fMRI): fMRI is a diagnostic test used to define the areas of the brain that are activated while performing any function, such as speech, walking, or eating. This is used to assess the damage that is caused to the brain. Activated areas would appear as a red or yellow signal. fMRI may also act as an adjunct tool preoperatively if the tumors are located in critical areas of the brain that could impede the functional ability of the patients.
Conclusion:
The prognosis of astrocytoma is variable depending on many factors. Therefore, imaging techniques play a crucial role in diagnosing and assessing tumors. Low-grade astrocytomas can be successfully treated with a better survival rate. However, a remission, if achieved, may be temporary or permanent.












