Introduction:
The thyroid gland is a small, butterfly-shaped gland located in front of the neck. It is a vital gland because the hormones it secretes regulates the metabolic functions of the body. The thyroid has indirect control over the entire body's functioning and development. Thyroid diseases have become extremely common, with the majority of them affecting women. Cancer affecting the thyroid gland is known as thyroid cancer. Though thyroid cancer is rare, it is considered the most common endocrine malignancy. Similar to thyroid diseases, thyroid cancer is most commonly seen in females. Yet, unlike other cancers, thyroid cancer has the best prognosis and is curable with successful treatment.
What Are the Symptoms of Thyroid Cancer?
Thyroid cancer is an extremely slowly developing disease; hence early disease does not show any signs and symptoms. As the disease progresses, the following signs and symptoms may develop:
-
A lump that can be felt in front of the neck or on either side of the throat.
-
Pain while swallowing.
-
Difficulty in talking or breathing.
-
Change in the tone of voice or sudden hoarseness.
-
Persistent coughing.
What Are the Risk Factors Associated With Thyroid Cancer?
Thyroid cancer develops when certain cellular changes occurs resulting from the mutation of the genetic material. The reason for these changes is debatable; however certain factors that can increase the risk of developing thyroid cancer are, as mentioned below:
-
Women are more at risk of developing thyroid cancer. Studies have attributed this to the role of estrogen hormone present in females.
-
High level of radiation exposure.
-
Hereditary genetic syndromes: Certain genetic syndromes pose an increased risk for the development of thyroid carcinoma. Certain thyroid cancer also is hereditary.
-
Iodine deficiency can also put individuals more at risk for thyroid cancer.
What Are the Different Types of Thyroid Cancer?
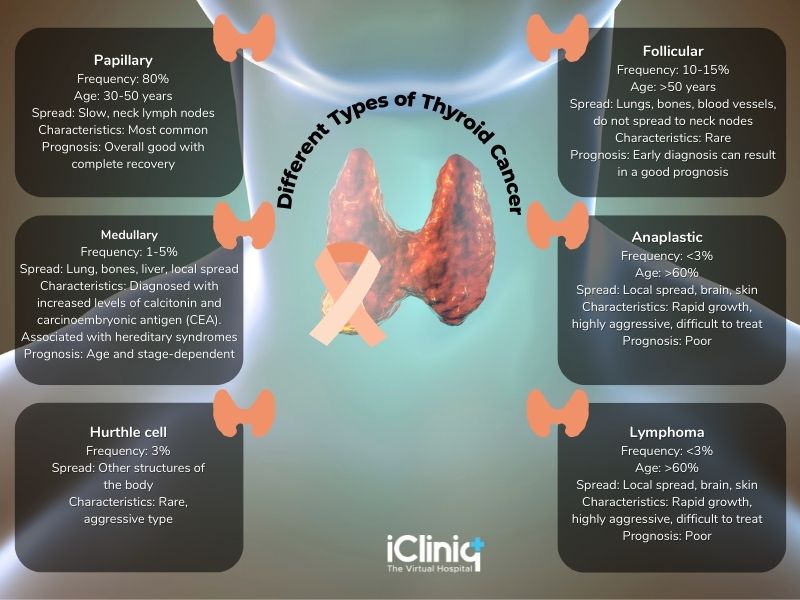
A pathological examination of a tissue sample from the thyroid helps in determining the types of thyroid cancer. The prognosis and treatment plan depends on these types.
What Are the Diagnostic Workups Required in Thyroid Cancer?
The diagnostic workup in thyroid cancer would be as below:
1. Physical Examination and Medical History:
-
A detailed medical history and physical examination of the lumps and other signs and symptoms will be the initial step.
2. Blood Tests:
-
Blood tests cannot diagnose thyroid cancer, but they can be used to determine the functioning of the thyroid gland.
-
Thyroid-stimulating hormones, T3 and T4 hormones, thyroglobulin, calcitonin, and carcinoembryonic antigen are most commonly assessed.
-
A high level of thyroglobulin is considered a post-surgical indicator for recurrence or remnant cancer cells. Thyroglobulin is produced by the thyroid tissues; hence after surgical removal of the thyroid gland, the thyroglobulin level should be ideally low.
3. Imaging Tests:
-
Ultrasound, X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) are all used to diagnose thyroid cancer and also to assess its spread.
4. Radioiodine Scans:
-
In this test, patients are administered a small quantity of radioactive iodine, and images are obtained with a specialized gamma camera. Thyroid cells have an increased affinity to iodine. Hence this iodine will be absorbed by thyroid tissue present anywhere in the body. This can be used in all subtypes of thyroid cancer except the medullary type, as they have a very low affinity to iodine.
5. Biopsy:
-
A biopsy can provide the confirmatory diagnosis and also the type of thyroid cancer.
What Is the Working Principle of a PET-CT Scan?
PET-CT scan determines the molecular functioning of the tissues. The radioactive material most commonly used in PET-CT scans is F-18 fluorodeoxyglucose (FDG) which is similar to a glucose molecule. This radioactive material accumulates in various tissues of the body depending on their metabolic activity. Since tumor cells are metabolically more active as they are rapidly dividing and their growth rate is exponential, they attract glucose at a higher rate. This results in an increased uptake of the radioactive material, which appears as a bright spot in the PET scan.
Though FDG is the commonly used radiotracer in PET scans, novel tracers are being evaluated for thyroid malignancies such as Iodine-124, 18F-DOPA, Iodine-131, or Iodine- 123.
Iodine-123:
-
Superior image quality.
-
Expensive.
-
Short half-life.
-
Restricted availability.
Iodine-131:
-
Inexpensive.
-
Easily available.
-
Poor resolution images.
Iodine-124:
-
Good half-life.
-
Superior sensitivity.
-
Better resolution images.
-
Highly sensitive to detect recurrence.
-
Many studies have 124I PET-CT to be comparable in terms of sensitivity and usefulness to FDG PET-CT.
What Is the Role of PET-CT in Thyroid Cancer?
PET scans have revolutionized the field of cancer diagnostics. PET scan uses a radioactive material that is injected into the body through a vein. Images would be taken with specialized cameras. PET scan determines the functioning of the organs and tissues based on the biochemical and metabolic activities occurring in the tissues. Assessing the changes in the tissue metabolic activity can help identify the disease earlier, even before any structural or anatomic changes have occurred, which may be seen only later in an imaging process.
A PET scan, when combined with CT, has proved even more efficient in diagnosing cancer and its spread. PET scan presents the functioning details of the tissues, whereas CT provides the anatomical and morphological details of the abnormalities. Thus a combined PET-CT can provide double diagnostic clarity, increasing the accuracy and efficacy of diagnosis.
PET-CT has a promising role in thyroid cancer. Though PET-CT is not a primary diagnostic tool in thyroid cancer, it has a great role as a prognostic indicator and also in recurrent thyroid cancer cases. It is also valuable to assess the metastatic spread of thyroid cancer. The indications are as discussed below:
1. Prognostic Indicator of Thyroid Cancer:
- PET-CT is proven to be an important prognostic marker in thyroid cancer.
- Thyroid cancer with high glucose metabolism and increased uptake of FDG indicates a poorly differentiated tumor, increasing malignant potentiality, and poor prognosis.
- Tumors with iodine affinity have low glucose metabolism and are hence well differentiated with a good prognosis.
2. In Recurrent Thyroid Cancer:
-
PET-CT plays a significant role in the follow-up of thyroid cancer patients who have undergone surgical treatment.
-
An elevated serum thyroglobulin level and negative radioiodine whole-body scan in post-surgical thyroid cancer patients is an indication of recurrence.
-
Patients with elevated serum thyroglobulin in the follow-up phase should be subjected to PET-CT to assess the recurrence.
3. In Metastatic Thyroid Cancer:
-
To check for the spread of cancer.
-
To look for cancer progression.
-
An elevated serum thyroglobulin level with abnormal whole-body radioiodine scans could indicate locoregional or distant metastases, which could be confirmed with the help of PET-CT.
4. In the Management of Thyroid Cancer:
-
To evaluate the response to treatment.
-
Cancers which have high FDG uptake are not likely to respond well to radioiodine treatment.
5. In High-Risk Cases:
-
To monitor patients with high-risk diseases.
-
To identify the site of the disease.
6. In Medullary and Anaplastic Thyroid Cancer:
-
PET-CT can be used to diagnose medullary thyroid cancer as radioiodine scans are not much useful in this type due to their low affinity for iodine.
-
To detect primary and metastatic anaplastic thyroid cancer.
-
Since medullary carcinomas arise from the C cells producing calcitonin, an increase in calcitonin or CEA levels is an indication for PET-CET to rule out medullary thyroid carcinoma.
How Is the Procedure Done?
-
Patients are advised to stop thyroid hormone before the PET scan procedure.
-
The thyroid-stimulating hormone (TSH) is accelerated so that the thyroid cancer cells can take up the radioactive material, thereby increasing the sensitivity of the test.
-
TSH can be stimulated by either withdrawing the thyroid hormone pill or by injecting a recombinant human TSH.
-
Patients will be injected with radioactive material into the vein. The patient may have to wait for 30 to 45 minutes for the radiotracer to disperse and be absorbed into the body.
-
Contrast material will also be injected through the intravenous (I.V) line.
-
Patients would be made to lie down in a PET-CT scanning machine where the images would be taken and processed.
-
After the procedure is completed, patients would be asked to drink plenty of water to expel the radioactive material from the body. The radioactive material is usually removed from the body via urine and stool.
Conclusion:
Thyroid cancer is considered to have an excellent prognosis and is completely treatable. Even recurrent thyroid cancer cases have a good prognosis as compared to others. Though PET-CT is not the prime diagnostic modality in thyroid cancer, it is proven to be the best prognostic indicator and an essential follow-up tool in patients with thyroid cancer.












