What Is a Croup?
Croup is a common acute respiratory tract infection seen in pediatric patients from six months to three years of age. It is a viral infection usually affecting the larynx, trachea, and at times the bronchi too. Hence, it is also known as acute laryngotracheitis and acute laryngotracheobronchitis. The viral infection results in inflammation of the larynx, trachea, and bronchi. This results in the development of inflammatory exudates and subsequent swelling of the subglottic area causing obstructive breathing and a barking cough. Croup is most often seen during the winter season, with an increased prevalence in boys.
What Causes Croup in Children?
-
It is mostly associated with a viral infection. The human parainfluenza virus is the most common virus associated with croup. Other viruses such as influenza virus, respiratory syncytial virus, coronavirus, adenovirus, and enterovirus may also result in croup.
-
Bacterial croup may also occur, but it is less common. The most common bacteria associated with croup are Mycoplasma pneumoniae and corynebacterium diphtheriae.
-
Exposure to certain allergens (allergy-producing substances) can also trigger croup.
-
Gastroesophageal reflux (when the contents of the stomach flow backward into the esophagus).
-
Croup usually spreads through direct contact either with an infected person or through droplet spread. The nose and nasopharynx are the entry points for the virus, which then spreads to the larynx and lungs.
-
Recurrent croup is associated with risk factors such as previous intubation history, premature kids, or toddlers below two years of age.
What Are the Symptoms of Croup in a Child?
-
The symptoms usually are abrupt onset.
-
Croup symptoms can aggravate at night times and with emotional distress in kids.
-
Barking cough and audible inspiratory stridor are characteristic features of croup.
-
Fever may or may not be present; if present, it is usually a low-grade fever.
-
Hoarseness and some respiratory distress may be seen.
-
Rhinitis (swelling inside the nose resulting in itching, runny nose, and nasal congestion).
-
In severe cases, the child may become cyanotic with deep shallow respirations.
How Can Croup Be Diagnosed?
The diagnosis of croup is essentially made based on clinical symptoms. The inspiratory stridor and barking cough are classic enough to conclude with the diagnosis of croup. Radiographic diagnosis is needed in cases with atypical symptoms or to rule out any other illness with overlapping features. The diagnostic workup in a child with suspected croup will be as follows:
1. History:
Detailed patient history can help doctors conclude the diagnosis of croup. The characteristic respiratory symptoms should be taken into diagnostic consideration. Also, a history of gastroesophageal reflux should be checked as reflux can be one of the causes of croup.
2. Physical Examination:
-
Children with mild cases present with just barking cough and hoarseness. Inspiratory stridor may be present at rest or mostly when the child is agitated.
-
In a severe case of croup, the child may seem to be in respiratory distress with stridor during inspiration and expiration.
-
Deep shallow respiration may be seen. Tachypnea, tachycardia, and cyanosis should be considered cautionary signs.
-
Respiratory rate and heart rate should also be assessed as they may be increased.
3. Imaging:
3.1 Plain Radiography:
-
Radiographs can act as an ancillary tool to aid the diagnosis of complicated or uncertain cases.
-
Patients will be subjected to lateral and anteroposterior X-rays (AP) of the neck and chest.
-
AP view will show the classic steeple sign (pencil point sign or wine bottle sign), which indicates the subglottic narrowing.
-
The lateral view would show a distended hypopharynx during inspiration. A lateral view is essential to differentiate epiglottitis as the appearance is the same as croup on the AP view.
3.2 Computed Tomography (CT):
-
CT is not routinely indicated. It is used to rule out conditions presenting as croup, such as foreign body aspiration, tracheal compression, or any anatomic conditions.
3.3 Magnetic Resonance Imaging (MRI):
-
Similar to CT, MRI is also used as an ancillary diagnostic aid for an alternative diagnosis.
3.4 Ultrasound (US):
-
The US is useful to rule out the differential diagnosis and also in cases requiring advanced diagnostic aids.
4. Laboratory Testing:
-
Laboratory testing is nonspecific and not of much importance to diagnose croup per se; however, it can add some value to the etiology and, thereby, the treatment aspect.
-
An increased white blood cell count (WBC) and lymphocytosis can help establish the viral etiology.
-
Pulse oximetry can be helpful in respiratory compromised patients to evaluate the need for supplemental oxygen.
What Are the Scoring Systems?
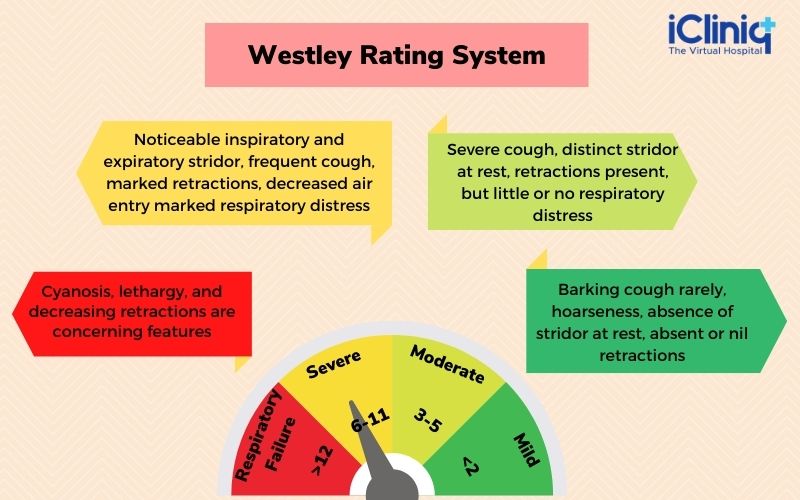
The most commonly used scoring system for croup is the Westley score which is as follows:
There are five factors to be considered.

With the above scores, a Westley rating system is generated, which is as below:
How Is Croup Treated?
Croup is a self-limiting condition that usually improves on its own. Most children feel better within three to seven days.
Mild Cases:
-
Adequate rest and plenty of hydration.
-
Acetaminophen for reducing the fever.
-
Keep the child’s head in an elevated position.
-
Try not to increase the child’s emotions as it could result in inspiratory stridor.
-
A humidifier or a cool-mist vaporizer can prevent drying up of the upper airway and thus facilitate breathing.
-
A steam bath can also help the child breathe comfortably.
Severe Cases:
-
Injectable steroids (a single dose of dexamethasone) are usually given.
-
Inhalation of Epinephrine by nebulizer.
-
Supplemental oxygen if needed.
-
Hospitalization is advised in cyanotic patients with increasing respiratory distress.
When to Seek Medical Advice?
-
Drooling saliva.
-
Stridor at rest.
-
Bluish discoloration of skin, mouth, or nails.
-
Increasing trouble while breathing.
-
Seizure.
-
Difficulty while speaking.
How to Prevent It?
-
Teach children correct hygiene practices. Washing hands properly.
-
Ask them to avoid sharing plates, glasses, and cutleries.
-
If your child is sick, make sure they stay at home.
-
Vaccinations against diphtheria and Haemophilus influenzae type b (Hib) can offer some protection; however, there are no vaccines currently against the parainfluenza virus.
What Is the Differential Diagnosis?
The inspiratory stridor (a whistling sound when breathing in) can be found in certain other conditions. Hence it is imperative to differentiate croup from other conditions:

Conclusion:
Croup is a self-limiting condition most commonly seen in children. Most often, the cases observed are mild and benefit from palliative measures and basic home care. Severe cases and those requiring hospitalization are uncommon, yet even they have an excellent recovery with timely treatment. The prognosis, by far, is considered to be excellent. However, children who remain symptomatic and have recurrent episodes of croup will require a detailed evaluation for appropriate treatment.












