Introduction:
The human body is made up of 206 bones. Although one of the strongest structures, they often succumb to systemic diseases. Bones mainly constitute calcium and phosphorus; any metabolic alterations in these elements can lead to pathologic changes in the bone. In addition, when bones become brittle, they tend to fracture easily after minimal trauma. Therefore, post-menopausal women and older adults are more susceptible to bone diseases. The health of bones is paramount in maintaining the structure of the body. Hence, it is essential to understand disorders of bone caused due to abnormal mineral metabolism.
What Are Metabolic Bone Diseases?
Metabolic bone disease is a broad term that describes disorders that affect bone strength due to bone mineral, vitamin D, mass, or structural alterations. Clinically, this might result in the weakening of bones, bone pain, and loss of bone height.
What Is Bone Actually Made Of?
Bone is mainly composed of organic and inorganic components.
-
Organic: Matrix composed of a fibrous protein (collagen) called osteoid.
-
Inorganic: Crystals of calcium and phosphate (hydroxyapatite).
-
Cells: Bone-forming and resorbing cells.
The bone constantly undergoes a series of changes throughout life. To maintain maximum bone strength, bones resorb and renew constantly. Typically, once the remodeling process is complete, the bone becomes rigid. However, in the case of metabolic bone diseases, maximum rigidity cannot be expected. This group of conditions tends to reduce bone density leading to noticeable changes. Common conditions affecting bone strength are described below.
What Are the Conditions That Influence Bone Metabolism?
The metabolic bone diseases can be broadly grouped as common and rare disorders. They are described in detail below:
A. Common Metabolic Bone Diseases:
1. Osteoporosis:
Osteoporosis is the most common metabolic bone disease that affects 200 million people worldwide. The disease is characterized by loss of bone mass and structural deterioration of bone tissue. As a result, individuals are susceptible to fractures of the spine, wrist, and hip. Women are more susceptible to this condition after menopause (natural cessation of the menstrual cycle). Men and women above the age of 50 years are at increased risk of osteoporosis by 13 percent and 40 percent, respectively. Osteoporosis can remain asymptomatic for years before patients begin to develop symptoms.
2. Rickets and Osteomalacia:
-
Rickets is a condition that occurs due to chronic vitamin D deficiency. The condition results in softening of the bones in children. Children may not get enough vitamin D due to a lack of sunlight, nutritious food, and certain genetic disorders related to absorption. Vitamin D is essential for the absorption of calcium and phosphorus, the two main components of bone. Rickets is characterized by pain, weakness in the muscles, delayed growth and motor skills, etc.
-
Osteomalacia is a condition that affects adults and is similar to rickets. Severe vitamin D deficiency forms weak and soft bones and affects the lower body. As a result, patients may experience dull pain, leg weakness, and walking difficulties as the disease progresses. In addition, systemic conditions such as kidney problems, surgeries, celiac disease (an autoimmune disorder), and certain drugs can lead to osteomalacia.
3. Hyperparathyroidism:
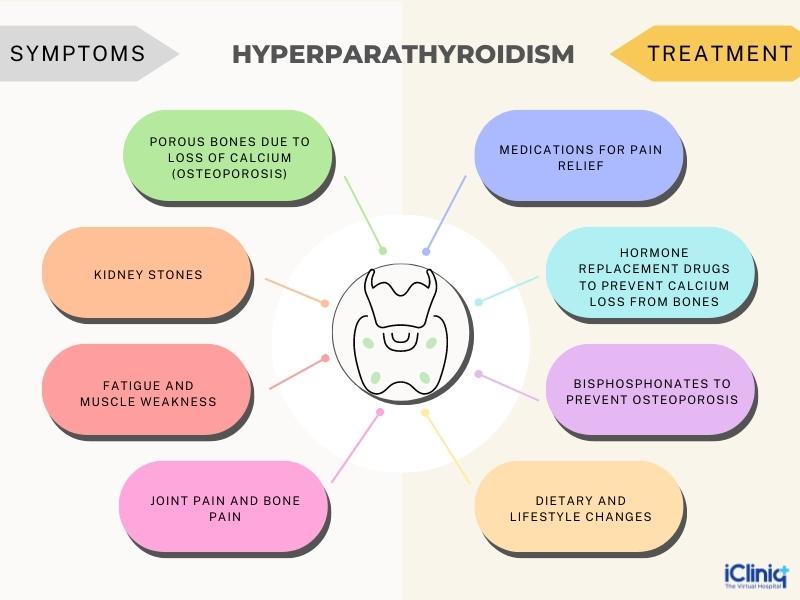
Parathyroid glands are pairs of pea-shaped glands located around the thyroid gland. They play a significant role in regulating calcium levels in the body by secreting parathyroid hormone. A higher level of parathyroid hormone in the body is called hyperparathyroidism. Hyperparathyroidism causes calcium loss from the bones rendering them brittle and weak. Additionally, there is increased calcium absorption and retention from the digestive tract and kidneys, respectively. Causes of hyperparathyroidism include vitamin D deficiency, kidney problems, tumors of the parathyroid, and certain genetic conditions.
B. Rare Metabolic Bone Diseases:
1. Paget’s Disease:
Paget’s disease is characterized by the replacement of old bone tissue with new, weaker, and brittle bone tissue. 2 percent to 3 percent of people above 55 years are diagnosed with Paget’s disease. It is a chronic condition that remains asymptomatic during the initial stages. Commonly affected bones include the pelvis, long bones, spine, and skull. The cause of Paget’s disease is not known; however, certain factors like age, genetic, and environmental factors increase the risk.
2. Hypophosphatasia:
Hypophosphatasia is a disorder characterized by soft bones due to poor skeletal mineralization. It occurs due to low serum alkaline phosphatase activity. It is experienced that the earlier the onset, the more severe the disorder. It is considered a childhood disease with a wide range of severity. It affects infants, children, and adults. There are six types of hypophosphatasia, namely benign prenatal, lethal perinatal, infantile, childhood, adult hypophosphatasia, and odontohypophosphatasia (affects only teeth).
What Are the Symptoms and Treatment of Metabolic Bone Disease?
1. Osteoporosis:

2. Rickets and Osteomalacia:

3. Paget’s disease:

4. Hyperparathyroidism:
5. Hypophosphatasia:

Conclusion:
Metabolic bone disease is a broad term that describes disorders that affect bone strength due to bone mineral, vitamin, mass, or structural alterations. The underlying conditions include osteoporosis, Paget’s disease, hyperparathyroidism, rickets, etc. Some of these conditions are inherited, and others are acquired. Symptoms of metabolic bone disease are bone pain, brittle bones, fractures, weakness, etc. Management and treatment depend on the underlying conditions. Hence, proper identification is required before carrying out any treatment.












